Summary
Objective
To determine the effect of intermittent pneumatic foot and calf compression on popliteal artery mean systolic blood flow in patients with intermittent claudication. The secondary objective was to determine the change in blood flow with posture.
Methods
This was a cross sectional study carried out on claudication patients at the Vascular Laboratory, Department of General Surgery, Kuala Lumpur Hospital, from January 2009 to August 2009. The effect of posture (supine to sitting to standing) and the effect of intermittent pneumatic compression (IPC) of the foot and calf on popliteal artery flow immediately and 10 minutes post compression were studied.
Results
Fifteen patients were studied. There was a consistent drop in flow from supine to sitting and to standing in all patients. Immediately after IPC application there was an increase in flow ranging from 29–335% (p < 0.05). Increase in flow was reduced but still sustained after 10 minutes with a flow range of 17–113 mL/minute with a median of 63 mL/minute (p < 0.05).
Conclusion
There is a significant reduction in popliteal artery mean systolic flow from supine to sitting and to the standing position, and popliteal artery flow is significantly increased after application of IPC and even persists after 10 minutes.
Keywords
intermittent claudication;intermittent pneumatic compression
1. Introduction
As early as the 1800s, physicians have experimented with the concept of improving blood circulation by exerting external pressure on the legs. In 1934, Reid and Herrmann1 proposed the use of alternating pressure and suction in what they called “PAVAEX” (passive vascular exercise) to treat various forms of lower limb arterial disease. Landis and Gibbon2 expanded this use of pressure–suction technique to include the treatment of ischemic limb, chronic ulcers, and claudication. It has been found recently that intermittent pneumatic compression of the foot and calf can generate a hemodynamic effect similar to that produced by a postural change from sitting to supine and reducing peripheral resistance. This can directly enhance arterial calf inflow and, if used for several consecutive weeks, improve lower limb hemodynamics.
Intermittent pneumatic compression is currently thought to be an effective means of augmenting arterial volume flow in the lower limbs of patients with peripheral vascular disease. Studies report a resting popliteal artery volume flow increases more than three times on application of intermittent calf compression3 and up to 84%4 when intermittent foot compression is applied. More recently interest has been focused on the potential clinical benefits that intermittent pneumatic compression might provide to patients with symptomatic peripheral vascular disease. It has been shown to improve the claudication distance and peripheral hemodynamics.5
Our center has previously studied the effects of IPC on the normal population,6 and as a follow up to that study, herein we have investigated the same effects on patients with intermittent claudication.
2. Patients and methods
This was a cross sectional study carried out over a period of eight months from January 2009 to August 2009 at the Vascular Laboratory of the Department of General Surgery, Kuala Lumpur Hospital. The participants were patients of all ages who presented to the Department of Vascular Surgery for treatment of intermittent claudication. Only those with stage II of Fontaines classification were included. All patients included in the study had a patent popliteal artery, with at least two crural vessel run off as determined by recent magnetic resonance imaging (MRA), computed tomography angiogram (CTA) or angiogram and a popliteal segment that was easily insonated by Doppler ultrasound.
The exclusion criteria included patients with congestive cardiac failure, chronic venous disease, leg trauma, swelling or ulcers, morbid obesity and those on vasoactive drugs (e.g., nifedipine). Ethics approval by CRC (Clinical research centre) of Hospital Kuala Lumpur was obtained for the study.
After obtaining informed consent, history and examination findings were entered into a standard form. Each participant was considered as a single patient and, in the event of bilateral claudication, in keeping with the inclusion criteria the worse limb in terms of severity was examined.
The popliteal artery was located using the Duplex Ultrasound machine (Philips HD11XE, Philips healthcare, 30000 minuteman road, Andover, United states) with a variable linear probe (12–3 MHz). B-mode real time ultrasound imaging was used to visualize the artery. The longitudinal real time image of the popliteal artery was confirmed three times before measurements of systolic flow were obtained. The diameter of the vessel was measured using the machines electronic calipers, after which the computerized data analysis provided by the machines software enabled instant calculation of the peak systolic flow of the popliteal artery in mL/minute.
Baseline popliteal artery mean systolic flow in the horizontal (supine) position was measured after a resting time of 10 minutes with the knee slightly flexed and the hip slightly rotated medially. The participant was then asked to sit at the edge of the bed for 10 minutes for flow stabilization before the sitting popliteal artery mean systolic flow was measured with both legs supported in a dependent, non-weight-bearing, position with the knee flexed in a comfortable position at about 45°, which also gave easy access for the Doppler probe to identify the artery. The patient was then asked to stand at the edge of the bed, and the systolic flow was measured after a flow stabilization of 10 minutes.
The patient was then asked to sit again and the intermittent pneumatic compression device was applied to the lower limb as describe previously.6
Statistical analysis was achieved using SPSS version 16.0 for Windows (SPSS Inc. 233 South Wacker Drive, 11th Floor, Chicago, IL). Wilcoxon signed rank test was used to compare the systolic flow after postural change and after IPC application.
3. Results
During the study period of 8 months, 15 patients were studied. There were 12 males and 3 female patients. All patients were over 40 years old.
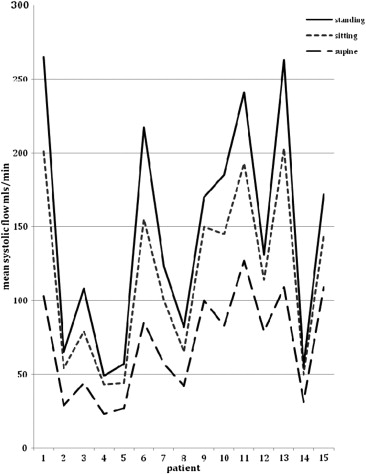
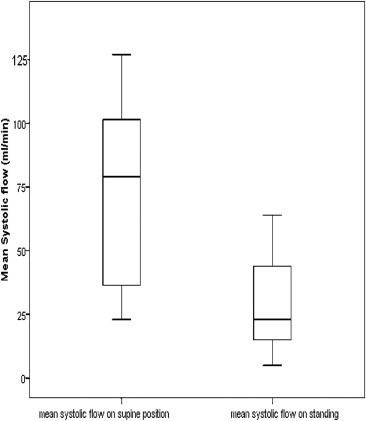
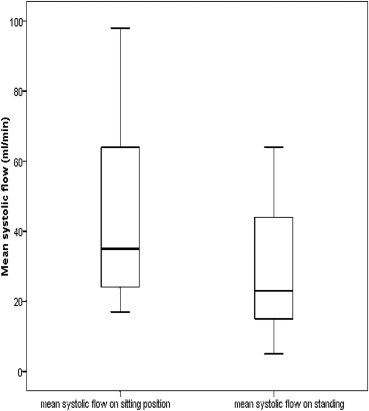
The popliteal artery mean systolic flow in the supine position was between 23–127 mL/minute with a median flow of 79 mL/minute. In the sitting position the popliteal mean systolic flow was between 23–98 mL/minute with a median flow of 35 mL/minute. There was a significant decrease in flow ranging from 5–68% with a mean of 32% (p < 0.05). In the standing position, the popliteal artery mean systolic flow was between 5–64 mL/minute with a median of 23 mL/minute. Once again there was a significant decrease in flow ranging from 17–74% with a mean of 40% (p < 0.05) - Figure 1, Figure 2 ; Figure 3.
|
|
|
Figure 1. Comparison of popliteal artery mean systolic flow in supine, sitting and standing positions. p value < 0.05 (Wilcoxon sign rank test). |
|
|
|
Figure 2. Box and Whisker plot showing the difference in popliteal artery mean systolic flow between supine and sitting positions (p < 0.05). |
|
|
|
Figure 3. Box and Whisker plot showing the difference in popliteal artery mean systolic flow between sitting and standing positions (p < 0.05). |
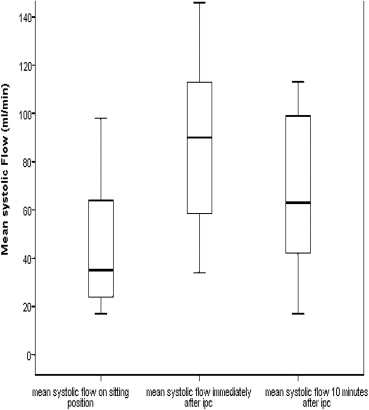
Immediately post IPC application, there was an increase in popliteal artery mean systolic flow in all 15 patients ranging from 29–335% with a median of 75%. The flow ranged from 34–146 mL/minute with a median of 90. Wilcoxon signed rank test gave a p value of < 0.05, showing that there was a significant increase in the popliteal artery blood flow between pre-application of IPC and immediately after application of IPC. At 10 minutes post IPC application, there were two patients that did not sustain a higher mean systolic flow ( Fig. 4). However, the rest were above baseline. The mean systolic flow ranged from 17–113 mL/minute with a median flow of 63 mL/minute. The Wilcoxon signed rank test again showed a p value of < 0.05 ( Fig. 5).
|
|
|
Figure 4. Comparison of popliteal artery mean systolic flow between sitting position, immediately after, and 10 minutes after IPC application. p value < 0.05 (Wilcoxon signed rank test). |
|
|
|
Figure 5. Box plot showing the difference in flow from baseline sitting to immediately after IPC application and 10 minutes after IPC application (p < 0.05). |
4. Discussion
Studies have documented that blood flow in the lower limbs decreases on assuming the erect position (sitting or standing).7 Henriksen postulated that the role of orthostatic changes of blood flow on patients with peripheral arterial disease (PVD) without rest pain displayed a similar vascular response to that seen in normal persons.8 The decrease of flow on dependency both in normal and claudication patients is called venoarteriolar response (VAR) and is attributed to the function of the peripheral sympathetic autoregulation. VAR is regulated by a sympathetic axon reflex, which is mediated by C-fibers. Owing to these fibers, elevation of the lower limb venous pressure as patients assume the dependent position, causes the arteriolar sphincters to contract, increasing the peripheral resistance to flow and decreasing arterial calf inflow. VAR is essential because it acts as a regulator of homeostasis and edema prevention.
Our study has demonstrated a statistically significant decrease in popliteal artery mean systolic flow from the supine to the sitting and then to the standing position. The reduction recorded ranged from 5–74% with a mean of 32%. Previous studies have shown that flow decreased by 17% on dependency (supine with legs hanging down) and by 47% on standing in normal persons.9 In a previous study carried out in our center, the popliteal artery peak systolic flow decreased by 23% ± 8% (692 mL/minute to 528 mL/minute) from supine to sitting position.6
More recent interest has focused on the potential clinical benefits that intermittent pneumatic compression (IPC) could provide to patients with symptomatic PVD. The beneficial role of IPC of the foot in deep vein thrombosis (DVT) prophylaxis is undisputable,10 and its role in peripheral vascular disease (PVD) is being widely studied. Understanding the mechanism involved in blood flow augmentation with IPC is important for its clinical application. The augmentation has been attributed to the increase of the arteriovenous gradient and decrease in peripheral resistance. As the tissue pressure increases on delivery of pneumatic impulses, the walls of the underlying veins collapse, projecting venous blood proximally to the calf and thigh, causing venous pressure to decrease transiently, until veins are refilled by forward flow from the arteries. The unbalanced hydrostatic pressure on the arterial side during this short transient post compression period is thought to be a major mechanism for the blood flow augmentation.11 Also postulated is a direct reduction in peripheral arterial resistance through a release of nitric oxide from shear stress in the venous radicals with IPC, the action of which by local diffusion on the adjacent arteriolar vessels causes them to dilate transiently with concurrent flow augmentation.12
Another proposed method by which peripheral resistance might be lowered by IPC involves the peripheral sympathetic autoregulatory reflexes. During pneumatic compression, venous pressure decreases to less than 25 mmHg and remains so for most of the deflation time. Under this condition, venoarteriolar response is not stimulated and pre-capillary sphincters do not constrict leading to an increase in blood flow instead.
In this study based on duplex ultrasound scanning, we confirmed that IPC of the lower limbs is an effective means of enhancing arterial calf inflow in claudication patients. Our findings on the flow effect of IPC are comparable with those reported previously. The mean systolic flow in the popliteal artery increased significantly (p < 0.05) after the application of IPC for 15 minutes. Immediately post application there was an increase of flow ranging from 29–335% with a flow of 34–146 mL/minute. A reading 10 minutes after application of IPC showed a slight reduction of flow, however it was still significantly higher than baseline (p < 0.05) and still represents a large increase in flow volume compared to the baseline sitting positing with an r value > 0.5. In clinical practice, patients are required to undergo longer sessions of IPC usage, and beneficial effects are usually seen after a period of sustained and continuous use.
Our findings on flow effect of IPC are compatible with those reported by Delis et al13 where a mean popliteal blood flow increase of 174.4% was achieved in claudication patients after IPC application. They also studied the difference in flow enhancement using foot and calf compression separately and concluded that the effects were greater with foot and calf compression.13
Morgan et al14 reported mean popliteal blood flow increase of 84% in arteriopaths (p < 0.03) on application of foot impulse compression. Flow decreased significantly in both groups on cessation of pump action. However, a level higher than baseline (p < 0.003) was still maintained up to 30 seconds after delivery of foot compression.
Prospective trials on the long-term effects of IPC in the management of PVD have been carried out and have shown promising results. Delis et al15 demonstrated a 100% increase in pain free maximal walking distance and post exercise ankle brachial index after 4 months of daily application of IPC with the clinical benefits being sustained for at least 1 year after treatment.
Montori et al16 investigated 107 patients with chronic limb ischemia, of whom 94.4% had leg ulcer and 25% had history of amputation. These patients used IPC at home on affected limbs for 6 hours daily. In 6 months complete wound healing and limb salvage was achieved in 40%. Over the duration of treatment, 64% had a significant increase in pulse volume amplitude, and all of these legs were salvaged.
The Mayo clinic reported their experience on 48 patients who underwent minor foot amputation during the years 1998–2004.17 Twenty patients in the control group required below knee amputations while only 10 patients (42%) from the treatment group required this. They concluded that the use of IPC as an adjunct to a standard wound care regiment in patients with chronic limb ischemia who undergo local foot amputation is associated with better wound healing and higher limb salvage.
Ramaswami et al18 found that IPC improves walking distance in patients with stable intermittent claudication and alleviates symptoms of limb ischemia. Also IPC should be the first treatment modality in patients with disabling claudication who are unfit for major reconstructive surgery.
In conclusion, our study has shown a significant increase in popliteal artery mean systolic flow in patients with intermittent claudication after the application of IPC to the foot and calf. There was also a reduction in popliteal artery mean systolic flow from the supine to sitting and to the standing position.
References
- 1 L.G. Herman, M.R. reid; The conservative treatment of arteriosclerotic peripheral vascular disease; Ann Surg, 100 (1934), pp. 750–760
- 2 E.M. Landis, J.H. Gibbon; The effect of alternate suction and pressure on blood flow to lower extremities; Ann Intern Med, 8 (1934), pp. 282–295
- 3 V.P. Bemmelen, M. Mattos, W.E. Fraught; Augmentation of blood flow in limbs with occlusive arterial disease by intermittent calf compression; J Vasc Surg, 19 (1994), pp. 1052–1058
- 4 K. Delis, N. Labropoulus, A.N. Nicolaides; Arterial calf inflow augmentation in PVD using intermittent pneumatic foot compression: effects on popliteal artery hemodynamics; Br J Surg, 19 (1994), pp. 1052–1058
- 5 K.T. Delis, A.N. Nicolaides, J.H.N. Wolfe; Peripheral sympathetic autoregulation in arterial calf inflow enhancement with intermittent pneumatic compression; Eur J Vasc Endovasc Surg, 22 (2001), pp. 317–325
- 6 R. Wilkins, H.H. Meyer, J. Litter; The effect of the dependent position upon blood flow in the limbs; Circulation, 11 (1950), pp. 373–379
- 7 K.T. Delis, A. Nicolaides, G. Stansby; Effect of posture on popliteal artery haemodynamics; Arch Surg, 135 (2000), pp. 265–269
- 8 O. Henriksen; Orthostatic changes of blood flow in subcutaneous tissue in patients with arterial insufficiency of the legs; Scand J Clin Lab invest, 34 (1974), pp. 103–109
- 9 G. Fanelli, M. Zasa, M. Baciarello, et al.; Systemic haemodynamic effects of sequential pneumatic compression of the lower limbs in a prospective study in healthy volunteers; J Clin Anesth, 20 (2008), pp. 338–342
- 10 T. Sculco, C. Cowell, W. Clifford; Prophylaxis against venous thromboembolic disease in patients having a total hip or knee arthoplasty; J Bone Joint Surg Am, 84 (3) (2002), pp. 466–477
- 11 K.T. Delis, A.N. Nicolaides, J.H.N. Wolfe; Improving walking ability and ankle brachial pressure indices in symptomatic peripheral vascular disease with intermittent pneumatic foot compression. A prospective controlled study with one year follow up; J Vas Surg, 31 (4) (2000), pp. 650–661
- 12 G. Mashour, R. Boock; Effects of shear stress on nitric oxide levels of human cerebral endothelial cells cultured in an artificial capillary system; Brain Res, 842 (1999), pp. 233–238
- 13 K.T. Delis, A.N. Nicolaides, N. Labropolos, G. Stansby; The effect of intermittent pneumatic foot versus simultaneous foot and calf compression on popliteal artery haemodynamics. A comparative study; J Vasc Surg, 32 (2000), p. 2
- 14 R.H. Morgan, J.V. Psaila, A.M. Gardner; Arterial flow enhancement by impulse compression; Vasc Surg, 25 (1991), pp. 8–15
- 15 K.T. Delis, A.N. Nicolaides, J.H. Wolfe; Peripheral sympathetic autoregulation in arterial calf inflow enhancement with intermittent pneumatic compression; Eur J Vasc Endovascular Surg, 22 (2001), pp. 317–325
- 16 V.M. Montori, S.T. Kavros, E.E. Walch, T.W. Rooke; Intermittent compressive pump for non healing wounds in patients with limb ischaemia. The Mayo clinic experience (1998–2000); Int Angiol, 21 (2002), pp. 360–366
- 17 S.J. Kavros, K.T. Delis, A.E. Turner, A.E. Voll, D.A. Liedl, T.W. Rooke; Improving limb salvage with intermittent pneumatic compression in patients with critical limb ischaemia: the Mayo Clinic experience (1998–2004); Int Angiol, 25 (2006), p. 105
- 18 G. Ramaswami, M. D'Alaya, L.H. Hollier, J. Mc Elhinney; Rapid foot and calf compression increases walking distance in patients with intermittent claudication. Result of a randomized study; J Vasc Surg, 41 (2005), pp. 794–801
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?