Summary
Objective
To evaluate the usefulness of the Alvarado scoring system in reducing the percentage of negative appendectomy in our unit.
Materials and methods
A cross-sectional study was conducted, comprising 110 patients, admitted to Surgical Unit I, Civil Hospital, Karachi, in 2011 with a preliminary diagnosis of acute appendicitis. Patients of both sexes and all age groups except younger than 10 years were included in the study and their Alvarado scores calculated, on the basis of which patients were divided into two groups: Group A (Alvarado score <6) and Group B (Alvarado score ≥6). The signs, symptoms, laboratory values, surgical interventions, and pathology reports of each patient were evaluated. Diagnosis was confirmed by histopathological examination. Sensitivity, specificity, and positive and negative predictive values were calculated.
Results
Out of 110 cases (79 males, 31 females), 31 belonged to Group A (28.2%) and 79 belonged to Group B (71.8%). Surgical procedures were performed in 98.2% of cases, along with conservative treatment. Final diagnosis by histopathology was confirmed in 77 cases (71.3%). The overall negative appendectomy rate was 28.7% (males: 28.2%, females: 30%). Sensitivity and specificity of the Alvarado scoring system were found to be 93.5% and 80.6% respectively. Positive and negative predictive values were 92.3% and 83.3%, respectively, and accuracy was 89.8%.
Conclusion
Alvarado score can be used effectively in our setup to reduce the incidence of negative appendectomies. However, its role in females was not satisfactory and needs to be supplemented by other means.
Keywords
Alvarado scoring;appendectomy;appendicitis
1. Introduction
Globally, acute appendicitis is a common surgical emergency1; 2; 3; 4; 5; 6; 7 ; 8 with a lifetime risk of 1 in 7,9 which means that 6% of the individuals suffer an attack during their lifetime.6 ; 7 The condition is difficult to diagnose especially during the early stages when the classical signs and symptoms are usually subtle.1 ; 6 Different disease processes mimic the diagnosis of acute appendicitis as there are a number of causes leading to pain in the right iliac fossa particularly in female patients.2 ; 10 It has been observed that many patients undergoing appendectomy prove to be negative on histopathology of the surgically removed appendix, which is the gold standard for diagnosis of appendicitis.11 Removing a normal appendix is a burden both on patients and health resources.3 However, early recognition of the condition and prompt operation have been the most important factors in reducing morbidity and possible mortality, length of stay, and cost of treatment.4
Several scoring systems have been used to aid in early diagnosis of acute appendicitis and its prompt management. These systems are valuable and valid instruments for discriminating between acute appendicitis and nonspecific abdominal pain.6 An example is the Alvarado scoring system, which is based on histopathology, physical examination, and a few laboratory investigations and is very easy to apply.2; 3; 4 ; 6 Definitive diagnosis can, however, be reached at surgery and after histopathology.2
The aim of our study was to evaluate the usefulness of Alvarado scoring system in reducing the percentage of negative appendectomy in our setup.
In our setup, the decision to operate the patient was taken by the senior physician provided the history and findings were consistent with the diagnosis of appendicitis. Alvarado score was calculated and then compared once the histopathological report was available, which is considered as a gold standard in diagnosis of acute appendicitis. Various scoring systems have been developed to help improve the diagnosis of acute appendicitis. many of them are difficult to apply in a clinical setting in emergency department primary care setting, especially in low resource countries. Alvarado score is simple, effective and can be easily applied. It provides an accurate and consistent triage tool for ruling out appendicitis and identifying those at higher risk. In one study at Cardiff the Alvarado score reduced the unusually high false positive appendectomy rate from 44% to 14%.1
2. Materials and methods
A cross-sectional study comprising consecutive patients (n = 110), admitted to Surgical Unit I, Civil Hospital, Karachi, with a preliminary diagnosis of acute appendicitis was conducted over a period of 1 year from January 2011 to December 2011. Patients of both sexes and all age groups, except those younger than 10 years, presented with pain in the right lower quadrant or paraumbilical pain shifting to the right iliac fossa and those who were clinically diagnosed as cases of acute appendicitis were included in the study and their Alvarado scores calculated.
The Alvarado scoring system is based on three symptoms, three signs, and two laboratory findings (Table 1).12
| Alvarado score | ||
|---|---|---|
| Symptoms | Migratory RIF pain | 1 |
| Nausea/vomiting | 1 | |
| Anorexia | 1 | |
| Signs | Right iliac fossa tenderness | 2 |
| Elevation of temperature | 1 | |
| Rebound tenderness RIF | 1 | |
| Laboratory findings | Leukocytosis | 2 |
| Neutrophilic shift to the left (>75%) | 1 | |
| Total score = 10 |
RIF = right iliac fossa.
On the basis of Alvarado score, patients were divided into two groups. Group A comprised patients with Alvarado score <6 and Group B those with Alvarado score ≥6. The decision for admission and surgical intervention was made by the surgeon independent of the score and was based on patients' history and clinical examination. Also, abdominal ultrasound was performed prior to appendectomy to exclude other pathologies. Management options include conservative treatment which was given to all patients and open or laparoscopic appendectomy, performed according to the surgeons choice. Gross operative findings were also endorsed and all specimens were subjected to histopathological assessment, which is considered the gold standard for final diagnosis of acute appendicitis.
Data were collected using a pretested questionnaire and analyzed using SPSS version 16 (SPSS Inc., Chicago, IL, USA). The reliability of Alvarado scoring system was assessed by calculating negative appendectomy rate which is defined as cases having no signs of inflammation on histopathology of surgically removed appendix.
3. Results
One hundred and ten patients with clinical features suggestive of acute appendicitis were included in the study. The largest age group was 10–20 years (n = 54, 49.1%). Among them, 71.8% (n = 79) were males and 28.2% (n = 31) were females. The symptoms at presentation included pain in right iliac fossa (98.2%), nausea and vomiting (75.5%), and anorexia (33.6%). Clinical examination revealed tenderness in right iliac fossa in 94 cases (85.5%), rebound tenderness in 70 cases (63.6%), and elevated temperature in 50 cases (45.5%). Laboratory analysis showed raised total leukocyte count in 70 cases (63.6%) with neutrophilia in 62 cases (56.4%).
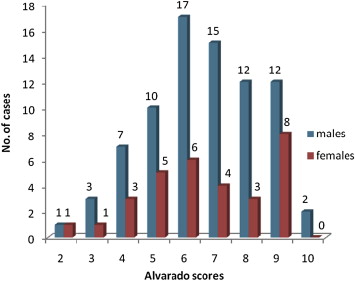
Of 110 patients, 31 belonged to Group A (28.2%) and 79 to Group B (71.8%). Details of Alvarado score in different patients are given in Fig. 1. Most patients presented with a score of 5 or 6 (n = 38), followed by a score of 7 or 8 (n = 34).
|
|
|
Figure 1. Sex-wise distribution of cases on the basis of the Alvarado score (n = 110). |
Ultrasound examination revealed that 55.5% (n = 61) of patients showed signs suggestive of appendicitis. Surgical procedures were performed in 98.2% of cases, along with conservative treatment of appendicitis, which was given to all the patients. Of 108 patients who underwent surgery, 57.4% (n = 62) were confirmed as having an inflamed appendix by the surgeon performing appendectomy, and perforated appendix was found in 9.2% of cases (n = 10). In patients found to have normal appendix at exploration, underlying pathology was right ovarian cysts (12.9%), mesenteric lymphadenitis (9.6%), pelvic inflammatory disease (9.6%), and right ureteric colic (9.6%). A list of findings at exploration in appendectomy is given in Table 2. In 13.6% (n = 15) of cases, no diagnosis was established. There are many causes of medical abdominal pain such as diabetic ketoacidosis and porphyrias that were not evaluated in these patients and might have resulted in “No diagnosis” in 15 cases. Of two patients who were not operated, one was subsequently diagnosed as having pelvic inflammatory disease and no diagnosis was established in the other.
| Findings | No. of patients (n) | % |
|---|---|---|
| Inflamed appendix | ||
| Acute appendicitis | 62 | 57.4 |
| Perforated appendix | 10 | 9.2 |
| Gangrenous appendix | 1 | 0.9 |
| Pus in appendix | 4 | 3.7 |
| Normal appendix | 31 | 28.7 |
| Right ovarian cyst | 4 | 12.9 |
| Pelvic inflammatory disease | 3 | 9.6 |
| Right ureteric colic | 3 | 9.6 |
| Mesenteric lymphadenitis | 3 | 9.6 |
| Worm infestation | 2 | 6.4 |
| Matted gut loops | 2 | 6.4 |
| Acute cholecystitis | 1 | 3.2 |
| Meckels diverticulum | 1 | 3.2 |
| No diagnosis | 12 | 38.7 |
Final diagnosis by means of histopathology was confirmed in 77 cases (71.3%; Table 3). The overall negative appendectomy rate was 28.7% (31 cases). The rates of negative appendectomies in males and females were 28.2% and 30% respectively. Sensitivity and specificity of the Alvarado scoring system were found to be 93.5% and 80.6% respectively. Positive and negative predictive values were 92.3% and 83.3%, respectively, and accuracy was 89.8%.
| Group | Histology positive (n) | Histology negative (n) | Total (n) |
|---|---|---|---|
| Group A | 5 | 25 | 30 |
| Group B | 72 | 6 | 78 |
Group A = Alvarado score <6; Group B = Alvarado score ≥6.
Of 31 patients in Group A, 21 were males and 10 were females. One patient was treated conservatively and 30 underwent appendectomy, but only five cases (16.7%) were confirmed positive on histopathological examination for acute appendicitis, giving the negative appendectomy rate of 83.3% in this group.
Of 79 patients in Group B, 58 were males and 21 were females. One patient was treated conservatively and the rest were operated, out of which 72 cases (92.3%) were confirmed as having acute appendicitis on histopathological examination, thus giving the negative appendectomy rate of 7.7% in this group. Surprisingly, negative appendectomy rate for females was 10%, which is considerably higher than that noted for males (6.8%).
Score-wise distribution of sensitivity revealed that patients with highest score (i.e., 9 or 10) had the highest percentage of sensitivity (100%). The sensitivity of the remaining high scoring groups is shown in Table 4.
| Score | No. of cases (n) | Sensitivity (%) |
|---|---|---|
| 9 or 10 | 22 | 100 |
| 7 or 8 | 34 | 94.1 |
| 5 or 6 | 38 | 60 |
4. Discussion
Acute appendicitis remains the most common abdominal condition requiring surgical intervention worldwide.8 Epidemiological studies have shown that appendicitis is more common in the age 10–20 years group.4 Our study also reveals high incidence in the age <20 years group, in concordance with Limpawattanisiri et al.4 Males were more frequently affected than females in our study, a finding in contrast with some studies.3 ; 5
The diagnosis of acute appendicitis still represents one of the most controversial tasks in general surgery, and can humble even the most experienced medical practitioner.4 This may be due to variable presentations of the disease and lack of a reliable diagnostic test.13 Surgical intervention early in the course of the disease to limit complications, leads to too many negative appendectomies being performed, with an associated mortality rate of 10%.14 The removal of a healthy appendix is associated with a greater risk of abdominal adhesions as compared to acute appendicitis.15 This contrasts with an increasing rate of appendiceal perforations associated with delayed surgical interventions for the purpose of increasing diagnostic accuracy at the opposite end of spectrum.4
An appropriate approach towards the diagnosis of acute appendicitis is reached mainly by good history and proper clinical examination.2 ; 3 However, it is reliable mainly for cases with classical presentation. Atypical cases present a diagnostic dilemma. Therefore, clinical diagnosis should be complemented with other diagnostic modalities such as ultrasound, computed tomography (CT), laparoscopy, and C-reactive protein levels to reduce negative appendectomy rate in equivocal cases.7; 16; 17 ; 18 Some studies found no help from CT in diagnosis of acute appendicitis presenting with equivocal examination.19; 20 ; 21 CT had changed the treatment plan in 58% patients according to one study4 and sensitivity and specificity with intravenous and oral contrast ranging from 91% to 98% and from 75% to 93%, respectively.19; 20; 22; 23; 24; 25 ; 26 An advantage is that it permits visualization of entire abdomen as an alternative diagnosis; this changes the treatment plan in 15% patients according to one study.22 CT has drawbacks, especially in resource-poor settings such as ours, as far as cost and availability are concerned, and it requires 2 hours to visualize oral contrast and during this time the appendix has a high chance to perforate.
To discriminate between acute appendicitis and nonspecific abdominal pain, various diagnostic scores have been advocated to reduce the frequency of negative surgeries,5; 13 ; 27 one of which is the Alvarado scoring system. Alvarado devised this in 1986, and it has been validated in adult surgical practice,12 by giving relative weight to specific clinical manifestations often found in such patients.4; 13 ; 15 It is simple, easy, extremely affordable, and relatively accurate in aiding clinical diagnosis especially in interpreting the extremes of score range.28 Various studies have shown promising results by incorporating this system in the diagnostic process with significant reduction in false negative cases.1; 2; 4 ; 6 In our study, 71.3% of cases (n = 77) were confirmed positive on histopathology, giving the overall negative appendectomy rate of 28.7%, in concordance with reports of 33.1% 7 and 33%,29 but in contrast with 14.7%4 and 11.49%,27 reported in other studies. The reason for the high rate of negative appendectomy in our setup may be that appendectomies were performed on almost all patients presented with conditions mimicking acute appendicitis. However appendiceal perforations were also seen in our study due to delayed diagnosis and referral in some cases. Perforation rate was 9.2% comparable to 7.8% and 9.4% in other studies. 3 ; 7
When considering the approaches to appendectomy, both open and laparoscopic procedures are appropriate for all patients. Patients treated with a laparoscopic appendectomy have significantly fewer wound infections, less pain, and a shorter duration of hospital stay, but higher rates of readmission, intra-abdominal abscess formation, and higher hospital costs.30 Outcome data on 235,473 patients with suspected acute appendicitis undergoing a laparoscopic or open appendectomy between 2000 and 2005 were obtained from the US Nationwide Inpatient Sample.31 The frequency of laparoscopic appendectomies increased from 32% to 58% over the period studied. The proportion of patients with uncomplicated appendicitis was significantly higher in the laparoscopic group (76% vs. 69%).
Patients undergoing a laparoscopic appendectomy for uncomplicated (e.g., imperforated, no abscess) acute appendicitis were significantly more likely to have a shorter mean hospital stay (1.5 days vs. 1.8 days), higher rates of intraoperative complications (odds ratio 2.61, 95% confidence interval 2.23–3.05), and higher costs (22%) compared with patients treated by an open appendectomy.
For patients with complicated appendicitis, defined as an appendiceal perforation or abscess, the laparoscopic approach was significantly associated with a shorter mean hospital stay (3.5 days vs. 4.2 days), higher rates of intraoperative complications (odds ratio 1.61, 95% confidence interval 1.33–1.94), and higher hospital costs (9%) compared to patients undergoing an open appendectomy for complicated appendicitis.
In our study, the overall sensitivity was 93.5%, similar to that reported by Limpawattanisiri et al4 and Shah et al.15 This high level of sensitivity (93.5%) suggests Alvarado score to be an effective diagnostic aid in acute appendicitis. Moreover, application of Alvarado score can provide high degree of positive predictive value (PPV) and high diagnostic accuracy. PPV of Alvarado score in our study was 92.3%, comparable with reported PPV of 83.5%,3 83.7%,4 ; 6 95.2%,7 and 85.4%.32 Diagnostic accuracy was 89.8%, which is consistent with 83.2% in Thailand.9
The gender-wise analysis of the Alvarado scoring system application revealed that this score falls disappointingly short of expectations in females, especially of child-bearing age, reporting a negative appendectomy rate of 30% in females as compared with males (28.2%). This finding is in concordance with other studies.4; 33 ; 34 Poor results in female patients were probably due to the fact that it is a clinically based diagnostic system and female patients with right iliac fossa pain have a wide range of differential diagnoses such as ectopic gestation, ovarian cyst torsion, salpingitis, and pelvic inflammatory disease.7; 13 ; 32 Similarly, diagnosis during pregnancy is made difficult by changes in position of appendix due to gravid uterus, nausea/vomiting, and raised leukocyte count during pregnancy.13 This implies the need for additional investigations such as pelvic examination, ultrasound, and other modalities to reduce negative appendectomy rate in this gender.35
Our study revealed significant differences in outcome for both the group of patients made on the basis of their calculated Alvarado scores. We noticed that in Group A, where Alvarado scores were less, the rate of negative appendectomy rate is high (i.e., 83.3%) in comparison with Group B where high Alvarado scores were associated with low frequency of negative appendectomies (7.7%). This is in concordance with Shah et al,15 who reported 71.4% versus 11.1% negative appendectomy rates in Groups A and B. This signifies that for high Alvarado scores the chances of having false positive cases are reduced, implying the need for further evaluation and observation in the <6 score group.14
It was noticed that although a high Alvarado score (≥ 6) provides an easy and satisfactory aid for the early diagnosis of acute appendicitis in the adult male population, the results are discouraging in the female population even in the group with scores ≥6, where the negative appendectomy rate was 10% as compared with males from the same group (6.8%). The reason may be the greater number of differential diagnosis in females even with high scores, resulting in over diagnosis of acute appendicitis.
We also noticed that even with high scores, clinical decision making for management of such patients varies according to the degree of clinical suspicion. In our study, patients with a score of 9 or 10 reported sensitivity of 100%, those with a score of 7 or 8 reported 94.1%, and with a score of 5 or 6 reported 60%, emphasizing the need for different management options in different groups of patients.
Therefore, the Alvarado scoring system should be used in clinical practice for determining the most probable management option in patients with different scores and clinical suspicion. However, the scoring system is not 100% reliable and diagnostically accurate, but it can be used as a complimentary aid to decide which management option is particularly suitable for the patients benefit.
In conclusion, the Alvarado score can be used effectively in our setup to reduce the incidence of negative appendectomies. The patients are not unduly exposed to risks of delay in intervention or significant increase in number of false negative cases. Its use is economical and can be applied easily even by junior surgeons with limited diagnostic facilities available to them. However its role in females was not satisfactory and needs to be supplemented by other means to improve the diagnostic accuracy. Ultrasound is the most commonly used investigation for this purpose. It helps to make prompt decision in suspected cases especially in patients at extreme of ages and females but it cannot be relied upon to the exclusion of the surgeons careful and repeated evaluation. Our recommendations are: false results are unlikely in patients with a high score (9 or 10) and no further investigation is needed; those with scores of 7 or 8 may require further investigations—especially female patients or those at age extremes; and those with scores of 5–6 may have the disease and further observation or investigations are needed.
References
- 1 T.D. Owen, H. Williams, G. Stiff, L.R. Jenkinson, B.I. Rees; Evaluation of Alvarado scoring in acute appendicitis; J R Soc Med, 85 (1992), pp. 87–88
- 2 A.G. Soomro, F.G. Siddiqui, A.H. Abro, S. Abro, N.A. Shaikh, A.S. Memon; Diagnostic accuracy of Alvarado scoring system in acute appendicitis; J Liaquat Univ Med Health Sci, 7 (2008), pp. 93–96
- 3 I. Khan, A.U. Rehman; Application of Alvarado scoring system in diagnosis of acute appendicitis; J Ayub Med Coll Abbotabad, 17 (2005), pp. 41–44
- 4 C. Limpawattanasiri; Alvarado score for the acute appendicitis in a provincial hospital; J Med Assoc Thai, 94 (2011), pp. 441–448
- 5 M.Y.P. Chan, C. Tan, M.T. Chiu, Y.Y. Ng; Alvarado score: an admission criterion in patients with right iliac fossa pain; Surgeon, 1 (2003), pp. 39–41
- 6 K. Singh, S. Gupta, P. Parga; Application of Alvarado scoring system in the diagnosis of acute appendicitis; JK Sci, 10 (2008), pp. 84–86
- 7 E.S. Kanumba, J.B. Mabula, P. Rambau, P.L. Chalya; Modified Alvarado scoring system as a diagnostic tool for acute appendicitis at Bugando Medical Centre, Mwanza, Tanzania; BMC Surgery, 11 (2011), pp. 1–5
- 8 M.S. Hanif, T.H. Tahir, I.A. Sheikh, M.Z. Ranjha; Acute appendicitis: gaining time in mass casualty scenario; Pak Armed Forces Med J, 3 (2010), pp. 1–6
- 9 M.A. Mardan, T.S. Mufti, I.U. Khattak, et al.; Role of ultrasound in acute appendicitis; J Ayub Med Coll Abottabad, 19 (2007), pp. 72–78
- 10 R. Yegane, H. Peyvandi, Hajinasrollah, N. Salehei, M. Ahmadei; Evaluation of modified Alvarado score in acute appendicitis among Iranian patients; Acta Medica Iranica, 46 (2008), pp. 501–506
- 11 K. Munir, J. Iqbal, U. Mushtaq, I. Ishaque, J. Mudassar, A. Khalid; Modified Alvarado scoring system in the diagnosis of acute appendicitis; APMC, 2 (2008), pp. 91–94
- 12 A. Alvarado; A practical score for the early diagnosis of acute appendicitis; Ann Emerg Med, 15 (1986), pp. 557–564
- 13 J. Phophrom, T. Trivej; The modified Alvarado score versus the Alvarado score for the diagnosis acute appendicitis; Thai J Surg, 26 (2005), pp. 69–72
- 14 N. Baidya, G. Rodrigues, A. Rao, S.A. Khan; Evaluation of Alvarado score in acute appendicitis: a prospective study; Internet J Surg, 9 (2007), pp. 1–6
- 15 S.W.A. Shah, C.A. Khan, S.A. Malik, A. Waqas, A.M. Tarrar, I.A. Bhutta; Modified Alvarado score: accuracy in diagnosis of acute appendicitis in adults; Prof Med J, 17 (2010), pp. 546–550
- 16 C. Schneider, A. Kharbanda, R. Bachur; Evaluating appendicitis scoring system using a prospective pediatric cohort; Ann Emerg Med, 49 (2007), pp. 778–784
- 17 S.M. Shafi, M.A. Malah, H.R. Malah, F.A. Reshi; Evaluation of modified Alvarado score incorporating the C-reactive protein in the patients with suspected acute appendicitis; Ann Nigerian Med, 5 (2011), pp. 6–11
- 18 P.L. Stephens, J.J. Mazzucco; Comparison of ultrasound and the Alvarado score for the diagnosis of acute appendicitis; Conn Med, 63 (1999), pp. 137–140
- 19 S.L. Lee, A.J. Walsh, H.S. Ho; Computed tomography and ultrasonography do not improve and may delay the diagnosis and treatment of acute appendicitis; Arch Surg, 136 (2001), pp. 556–562
- 20 J.J. Hong, S.M. Cohn, A.P. Ekeh, et al.; A prospective randomized study of clinical assessment versus computed tomography for the diagnosis of acute appendicitis; Surg Infect (Larchmt), 4 (2003), pp. 231–239
- 21 K.T. Morris, M. Kavanagh, P. Hansen, M.H. Whiteford, K. Deveney, B. Standage; The rational use of computed tomography scans in the diagnosis of appendicitis; Am J Surg, 183 (2002), pp. 547–550
- 22 J.G. Schuler, M.J. Shortsleeve, R.S. Goldenson, J.M. Perez-Rossello, R.A. Perlmutter, A. Thorsen; Is there a role for abdominal computed tomographic scans in appendicitis?; Arch Surg, 133 (1998), pp. 373–376
- 23 A. Ceydeli, S. Lavotshkin, J. Yu, L. Wise; When should we order a CT scan and when should we rely on the results to diagnose an acute appendicitis?; Curr Surg, 63 (2006), pp. 464–468
- 24 J. Perez, J.E. Barone, T.O. Wilbanks, D. Jorgensson, P.R. Corvo; Liberal use of computed tomography scanning does not improve diagnostic accuracy in appendicitis; Am J Surg, 185 (2003), pp. 194–197
- 25 D. Gaitini, N. Beck-Razi, D. Mor-Yosef, et al.; Diagnosing acute appendicitis in adults: accuracy of color Doppler sonography and MDCT compared with surgery and clinical follow-up; AJR Am J Roentgenol, 190 (2008), pp. 1300–1306
- 26 T. Terasawa, C.C. Blackmore, S. Bent, R.J. Kohlwes; Systematic review: computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents; Ann Intern Med, 141 (2004), pp. 537–546
- 27 K.A. Malik, M.R. Sheikh; Role of modified Alvarado score in acute appendicitis; Pak J Surg, 23 (2007), pp. 251–253
- 28 K.I. Ahmad, A.S. Shamsul, M.S. Ismail; The relationship between Alvarado score and pain score in managing adult acute appendicitis in emergency department; J Surg Academia, 1 (2011), pp. 15–29
- 29 J.R. Izbicki, W.T. Knoefel, D.K. Wilker, et al.; Accurate diagnosis of acute appendicitis: a retrospective and prospective analysis of 686 patients; Eur J Surg, 158 (1992), pp. 227–231
- 30 S. Sauerland, T. Jaschinski, E.A. Neugebauer; Laparoscopic versus open surgery for suspected appendicitis; Cochrane Database Syst Rev (2010) CD001546
- 31 E. Sporn, G.F. Petroski, G.J. Mancini, J.A. Astudillo, B.W. Miedema, K. Thaler; Laparoscopic appendectomy—is it worth the cost? Trend analysis in the US from 2000 to 2005; J Am Coll Surg, 208 (2009), pp. 179–185
- 32 S. Nizamuddin, K.A. Samo, M.H. Mangi, S.U. Rehamn; Protocol based management of acute right iliac fossa pain to improve the diagnostic accuracy; Medical Channel, 15 (2009), pp. 101–104
- 33 G. Fenyö, G. Lindberg, P. Blind, L. Enochsson, A. Oberg; Diagnostic decision support in suspected acute appendicitis: validation of a simplified scoring system; Eur J Surg, 163 (1997), pp. 831–838
- 34 M. Kalan, D. Talbot, W.J. Cunliffe, A. Rich; Evaluation of the modified Alvarado score in the diagnosis of acute appendicitis: a prospective study; Ann R Coll Surg, 76 (1994), pp. 418–419
- 35 U.K. Shrivastava, A. Gupta, D. Sharma; Evaluation of the Alvarado score in the diagnosis of acute appendicitis; Trop Gastroenterol, 25 (2004), pp. 184–186
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?