(Created page with "==Summary== ====Background==== Minimally invasive liver resection is feasible for select patients. The flexibility of robotic surgical instruments improves the possibility o...") |
m (Scipediacontent moved page Draft Content 678748452 to Wu et al 2014b) |
(No difference)
| |
Latest revision as of 12:32, 26 May 2017
Summary
Background
Minimally invasive liver resection is feasible for select patients. The flexibility of robotic surgical instruments improves the possibility of minimally invasive liver resection, even in challenging major liver resection.
Materials and methods
We accumulated 69 patients who underwent pure laparoscopic liver resection from 2007 to 2011, and 52 patients who underwent robotic-assisted minimally invasive liver resection in 2012. The patients' characteristics, surgical procedures, and perioperative parameters were described and compared between these two groups.
Results
In 2012, we performed 56 robotic hepatobiliary procedures, which included 52 (92%) robotic-assisted minimally invasive liver resection procedures. Under the assistance of a robotic system, we increased the number of patients undergoing minimally invasive liver resection by more than twofold, and we increased the percentage of minimally invasive surgery for patients with fresh hepatocellular carcinoma, compared to our laparoscopic group (44% vs. 15%, respectively). We also increased the percentage of major hepatectomy for minimally invasive liver resection by a robotic approach (39% vs. 15%) with a comparable conversion rate (5%) and morbidity (8%), compared to the laparoscopic group. We can even perform a challenging living donor liver harvest procedure with a robotic-assisted minimally invasive approach.
Conclusion
Robotic assistance increased the percentage of minimally invasive liver resections and the percentage of major minimally invasive liver resections with comparable perioperative results. Robotic-assisted minimally invasive liver resection is feasible, but its role needs more accumulated experience to clarify.
Keywords
minimally invasive liver resection;robotic hepatectomy
1. Introduction
Minimally invasive surgery has been applied widely for many surgical procedures. It has the advantages of a shorter hospital stay, less blood loss, less adhesion, and better postoperative recovery. Liver resection requires advanced surgical technique, especially for the cirrhotic liver. Therefore, the progression of minimally invasive liver resection is relatively slow, compared with other surgical procedures. In 1992, the first case report of minimally invasive liver resection was reported; however, in 2002, the first series report of minimally invasive liver resection was published. Some challenging major liver resection procedures can be performed by experienced surgeons because of the accumulation of surgical experience and improvements in surgical instruments. However, there are some problems to overcome prior to the popular application of minimally invasive surgery for liver resection. The flexibility of surgical instruments is very important and convenient for minimally invasive surgery, especially during tissue dissection, suturing, and reconstruction. The instruments of traditional laparoscopic surgery do not have much flexibility when they are applied into the abdominal cavity. This limits the application of minimally invasive surgery for challenging procedures.
In the past decade, the robotic surgical system has been applied in several different minimally invasive surgical procedures with the potential added advantages of instrument flexibility, three-dimensional (3D) surgical version, and stability, compared to tradition laparoscopic surgery. However, the feasibility and safety have not been well demonstrated. We tried to identify the potential application of robotic-assisted minimally invasive liver resection.
2. Materials and methods
In 2007, we established a program of minimally invasive liver resection at the National Taiwan University Hospital (Taipei, Taiwan). By the end of 2011, we had performed 69 laparoscopic hepatectomies. After the installation of our first robotic surgical system (da Vinci Si, intuitive com., USA) in January 2012, we applied a robotic system for minimally invasive liver resection. By the end of 2012, we proceeded to perform hepatobiliary surgical procedures, which included 52 (92%) robotic hepatectomies in 56 patients. We analyzed retrospectively the patient characteristics, surgical indications, surgical procedures, and perioperative outcomes between our two different periods (laparoscopic vs. robotic). The Student t test was applied for the statistics analysis. A value of p < 0.5 defined the statistical difference.
3. Results
3.1. Patient position, operative room setting, and port insertions for robotic hepatectomy
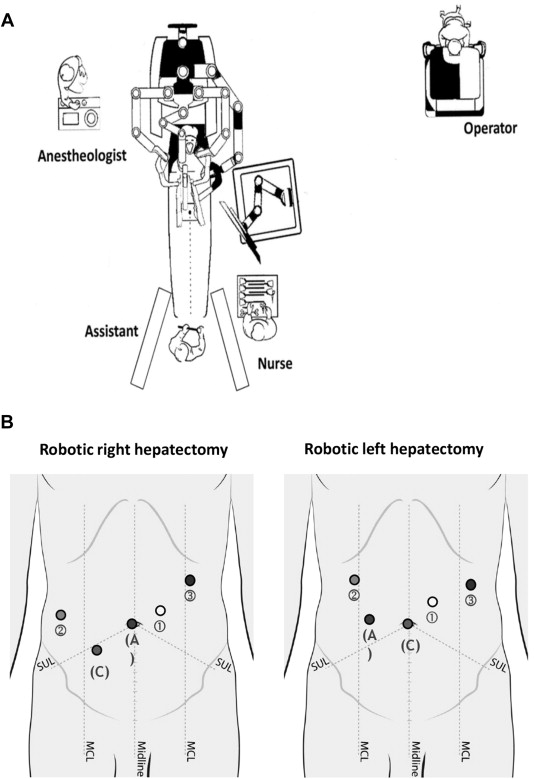
We placed the patient in the supine position and the reverse Trendelenburg position with both legs separated. We tilted the table 30 degrees to the left side if the lesion was located in the right lobe. The table assistant stood on the right side of patient or between the patients legs. We applied four robotic arms to perform robotic hepatectomy. The patient cart came from the head of the patient and the operator sat on the surgeons console a few steps away (Fig. 1A). For the trocar port placement for the robotic right hepatectomy, we first created the 12-mm assistant port through the umbilicus, followed by a second arm port over the right anterior axillary line, the 12-mm camera port between the second arm, and the assistant port at least 8 cm away from the second arm, the third arm port over the left anterior axillary line and subcostal area, and the first arm port between the assistant and the third arm ports at least 8 cm away from the third arm port. We switched the camera and the assistant port, and rotated clockwise the axis of the other ports for the robotic left hepatectomy (Fig. 1B). We then put the surgical specimen into an endobag and retracted it via the umbilical wound extension or the suprapubic wound.
|
|
|
Figure 1. (A) Typical operating room set up for robotic hepatectomy. (B) Port placements for robotic hepatectomy. A = assistant port; C = camera port; MCL = middle clavicle line; SUL = spinal umbilical line. |
3.2. Case number of minimally invasive liver resection and percentage of minimally invasive liver resection for patients with fresh hepatocellular carcinoma
We accumulated 69 patients who underwent minimally invasive liver resection by laparoscopic approach from 2007 to 2011 (Fig. 2A). However, the case numbers were limited, even after overcoming the learning curve in the first 2 years. We strictly selected suitable patients for laparoscopic liver resection. Sometimes we were not confident in using the laparosopic instruments to perform challenging major liver resection. In January 2012, we initiated a program of robotic liver resection after installing the da Vinci Si surgical system, and performed 56 robotic hepatobiliary surgical procedures, which included 52 (93%) patients who underwent robotic liver resection. The case number of minimally invasive liver resection increased by more than twofold after the assistance of the robotic surgical system. In our laparoscopic period, the percentage of minimal liver resection for patients with fresh hepatocellular carcinoma (HCC) was approximately 15% (10–23%); it increased to 44% in our robotic period (Fig. 2B).
|
|
|
Figure 2. (A) Case number of minimally invasive surgery (MIS) for liver resection. (B) The percentage of MIS for fresh hepatocellular carcinoma (HCC). |
3.3. Patients' disease characteristics and surgical procedures for minimally invasive liver resection
The disease characteristics included 63% malignancy in our laparoscopic liver resection group and 75% malignancy in our robotic liver resection group. Most malignant cases were HCC (59% in the laparoscopic resection group and 73% in the robotic liver resection group) (Table 1). We also performed one living donor left lobe harvest via the robotic approach. The percentage of major liver resection (i.e., more than three segmentectomies) was 15% in our laparoscopic series, and increased to 39% in our robotic series (Table 2).
| Indications | Laparoscopic liver resection (n = 69) | Robotic liver resection (n = 52) |
|---|---|---|
| HCC | 41 (59) | 38 (73) |
| FNH | 13 (19) | 7 (14) |
| Hemangioma | 7 (10) | 2 (4) |
| Metastasis | 3 (4) | 1 (2) |
| Adenoma | 1 (1) | |
| Angiomyolipoma | 1 (1) | |
| Dysplasia | 3 (4) | |
| Living donor | 1 (2) | |
| Klatskin tumor | 1 (2) | |
| Intrahepatic stone | 2 (4) |
Data are presented as n (%).
FNH = focal nodular hyperplasia; HCC = hepatocellular carcinoma.
| Type of resection | Laparoscopic liver resection (n = 69) | Robotic liver resection (n = 52) |
|---|---|---|
| Wedge | 7 (10) | |
| One segmentectomy | 21 (30) | 8 (15) |
| Two segmentectomy | 31 (45) | 24 (46) |
| Three segmentectomy | 2 (3) | 1 (2) |
| Left lobectomy | 6 (9) | 6 (12) |
| Right lobectomy | 2 (3) | 12 (23) |
| Left+S5+S6 segmentectomy | 1 (2) |
Data are presented as n (%).
3.4. Comparison of minimally invasive liver resection for patients with fresh HCC between the laparoscopic and robotic approach
We compared the perioperative parameters for our patients with fresh HCC between the laparoscopic approach and the robotic approach. The tumor size was larger in our robotic group (3.4 cm vs. 2.5 cm, respectively), and the percentage of liver resection of more than two segments was statistically increased in our robotic group (78% vs. 37%, respectively). However, we obtained a longer operation time and greater blood loss in our robotic group (Table 3). We performed two conversions (5%) to laparotomy in our robotic liver resection for HCC because of uncontrolled bleeding from the right hepatic vein (HV) and malignant hyperthermia. We did not perform any conversions after our first 20 robotic liver resections. We had three (8%) minor complications in our robotic liver resection for fresh HCC, including bile leakage,1 subphrenic abscess,1 and pneumonia.1 All patients improved after conservative treatment. We did not have any surgical mortality in our minimal liver resection.
| Robotic (n = 38) | Laparoscopy (n = 41) | p | |
|---|---|---|---|
| Age (y) | 60.9 ± 14.9 | 54.1 ± 14 | 0.04∗ |
| Sex (M:F) | 32:6 | 28:13 | NS |
| Tumor size (cm) | 3.4 ± 1.7 | 2.5 ± 1.6 | 0.02∗ |
| Operative method (≥2 segments) | 28 (78) | 15 (37) | 0.04∗ |
| Operating time (min) | 380 ± 166 | 227 ± 80 | 0.04∗ |
| Blood loss (mL) | 325 ± 480 | 173 ± 165 | 0.03∗ |
| Conversion (rate) | 2 (5) | 5 (12.2) | NS |
| Postoperative stay (d) | 7.9 ± 4.7 | 7.2 ± 4.4 | NS |
| Mobility | 3 (8) | 4 (10) | NS |
| Mortality | 0 | 0 | NS |
| Follow-up (mo) | 5.1 ± 2.8 | 26.6 ± 13.3 |
Data are presented as n (%) or mean ± SD.
∗Indicates a statistically significant difference (p < 0.05).
NS = not significant.
4. Discussion
Minimally invasive surgery has been developed as the preferred strategy for many surgical procedures with documented better postoperative recovery. The liver resection via a minimally invasive approach demands highly technical skill, but it progressed quickly and accumulated more than two thousand patients in the past 5 years. Laparoscopic hepatectomy, based on a world series review, is a safe procedure with acceptable morbidity and mortality for minor and major hepatic resection in experienced hands. In addition, the oncological results after laparoscopic hepatectomy for HCCs and for liver metastasis are comparable to open liver resection in selected patients. However, most procedures for laparoscopic hepatectomy were minor hepatectomies. The percentage of major liver resection by laparoscopic approach is only 16%.1 The Louisville Statement for laparoscopic liver surgery also describes the safety and feasibility of this procedure. The authors of the statement made a consensus that lateral segmentectomy should be performed routinely by a laparoscopic approach, but major liver resection by laparoscopic approach should be performed by experienced experts.2 Some of the limitations with laparoscopic major liver resection result from the flexibility of surgical instruments.
Since 2000, the robotic surgical system has been applied to assist minimally invasive surgery. It has added advantages such as flexibility and stability of surgical instruments, and a 3D and amplified surgical version. There are more than 75% of robotic surgical procedures used in gynecology and urology. The experience of robotic surgery in the other field is limited. Since 2007, the application of robotic surgery for liver resection has been reported. The feasibility, safety, and perioperative outcomes are comparable with those of laparoscopic liver resection.3; 4; 5 ; 6 There are approximately 200 reported robotic liver resections with a 4.6–7.8% conversion rate and 11.8–20.3% morbidity. No perioperative mortality was reported after robotic liver resection. Approximately 70% of robotic liver resection are performed because of malignant diseases such as liver metastasis (37%) and HCC (24%). The percentage of major liver resection by the robotic approach increased to 33%.7 ; 8 The robotic surgical system has also been applied to challenging minimally invasive surgery such as solid organ transplantation in the kidney, liver, and pancreas.9 ; 10 A proven advantage is decreased surgical infection rate in obese kidney recipients, which reflect superior outcomes for immunocompromised patients.11 The robotic surgical technique has been applied in the recipients operation and in the living donor harvest. Even the challenging right hepatectomy for a living donor can be performed by a robotic approach.12
In our experience with minimally invasive liver resection, we initially applied a laparoscopic approach. However, suitable candidates for minimally invasive liver resection are limited. Only 15% of our patients operated on for fresh HCC underwent a minimally invasive approach. In addition, the minimally invasive major liver resection accounted for 15% in our laparoscopic experience. The rigidity of laparoscopic instruments sometimes caused us to hesitate in deciding to use a minimally invasive approach, especially for a challenging major liver resection. We tried to overcome these limitations by robotic assistance. We increased the case number of minimally invasive liver resection by twofold and the percentage of minimally invasive approach for patients with fresh HCC during our robotic period. We also increased the percentage of major hepatectomy from 15% to 44% under the assistance of the robotic system with a conversion rate (5%) and morbidity (8%) comparable to those of laparoscopic liver resection. We had greater blood loss and longer operation time in the robotic group, which may have been contributed to by the larger tumor size and more major liver resection.
In conclusion, robotic-assisted minimally invasive liver resection is a feasible procedure. With the assistance of the robotic system, we increased the percentage of minimally invasive surgery for our patients with fresh HCC, and the percentage of major liver resection by a minimally invasive approach. The challenging liver harvest operation from a living donor also can be performed by a minimally invasive approach under the assistance of the robotic system. We have to accumulate more experience to clarify the role of the robotic system in minimally invasive liver resection.
References
- 1 K.T. Nguyen, T.C. Gamblin, D.A. Geller; World review of laparoscopic liver resection: 2804 patients; Ann Surg, 250 (2009), pp. 745–758
- 2 J.F. Buell, D. Cherqui, D.A. Geller, et al.; The international position on laparoscopic liver surgery: the Louisville Statement, 2008; Ann Surg, 250 (2009), pp. 825–830
- 3 P.C. Giulianotti, A. Coratti, F. Sbrana, et al.; Robotic liver surgery: results for 70 resections; Surgery, 149 (2011), pp. 29–39
- 4 E.C. Lai, C.N. Tang, M.K. Li; Robot-assisted laparoscopic hemi-hepatectomy: technique and surgical outcomes; Int J Surg, 10 (2012), pp. 11–15
- 5 P.C. Giulianotti, F. Sbrana, A. Coratti, F.M. Bianco, P. Addeo, N.C. Buchs; Totally robotic right hepatectomy: surgical technique and outcomes; Arch Surg, 146 (2011), pp. 844–850
- 6 G.H. Choi, S.H. Choi, S.H. Kim, et al.; Robotic liver resection: technique and results of 30 consecutive procedures; Surg Endosc, 26 (2012), pp. 2247–2258
- 7 A.D. Carr, M.R. Ali, V.P. Khatri; Robotic hepatobiliary surgery: update on the current status; Minerva Chir, 68 (2013), pp. 479–487
- 8 C.M. Ho, G. Wakabayashi, H. Nitta, N. Ito, Y. Hasegawa, T. Takahara; Systemic review of robotic liver resection; Surg Endosc, 27 (2013), pp. 732–739
- 9 I. Tzvetanov, L. Bejarano-Pineda, P.C. Giulianotti, et al.; State of the art of robotic surgery in organ transplantation; World J Surg, 37 (2013), pp. 2791–2799
- 10 U. Boggi, S. Signori, F. Vistoli, et al.; Laparoscopic robot-assisted pancreas transplantation: first world experience; Transplantation, 93 (2012), pp. 201–206
- 11 J. Oberholzer, P. Giulianotti, K.K. Danielson, et al.; Minimally invasive robotic kidney transplantation for obese patients previously denied access to transplantation; Am J Transplant, 13 (2013), pp. 721–728
- 12 P.C. Giulianotti, I. Tzvetanov, H. Jeon, et al.; Robot-assisted right lobe donor hepatectomy; Transpl Int, 25 (2012), pp. e5–e9
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?