(Created page with "A 60-year-old man was hospitalized because of acute diverticulitis complicated with ''Bacteroides fragilis'' bacteremia. The computed tomography (CT) scan showed cecal divert...") |
m (Scipediacontent moved page Draft Content 968440010 to Tseng Chen 2015a) |
(No difference)
| |
Latest revision as of 12:01, 15 May 2017
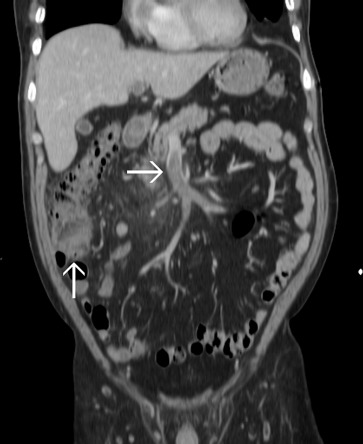
A 60-year-old man was hospitalized because of acute diverticulitis complicated with Bacteroides fragilis bacteremia. The computed tomography (CT) scan showed cecal diverticulitis with superior mesenteric vein (SMV) thrombosis ( Fig. 1 ). At that time, he received parenteral antibiotics for 2 weeks and then oral antibiotics for 1 week after discharge. Nine days later, he presented to our emergency department with progressive abdominal pain and fever. CT scan demonstrated improved diverticulitis but progressive local peritoneal inflammation around the SMV thrombosis (Fig. 2 ).
|
|
|
Figure 1. The upward arrow indicates cecal diverticulitis and the rightward arrow indicates superior mesenteric vein thrombosis. |
|
|
|
Figure 2. The upward arrow indicates the improved diverticulitis and the rightward arrow indicates the progressive thrombophlebitis. |
Septic thrombophlebitis is venous thrombosis-associated inflammation with positive blood culture results. It is an uncommon complication of intra-abdominal infections such as cholangitis, diverticulitis, and appendicitis. Septic thrombophlebitis carries a high mortality risk if patients do not receive adequate treatment [1] . Septic thrombophlebitis may involve superficial veins or deep veins such as portal venous system. The clinical presentation and laboratory examination of thrombophlebitis are nonspecific, which may delay diagnosis [2] . The most frequently isolated bacteria are Escherichia coli , Bacteroides fragilis , Proteus mirabilis , Klebsiella pneumoniae , and Enterobacter spp. [3] . Ultrasound, magnetic resonance imaging, and CT scans have been used in diagnosis. The latter two imaging techniques may be better than ultrasound because they can also identify the source of infection [1] ; [2] . Nephrotic syndrome, myeloproliferative neoplasms, paroxysmal nocturnal hemoglobinuria, and antiphospholipid syndrome are also possible causes of abdominal vein thrombosis [4] ; [5] . Therefore, further tests may be considered according to the patients clinical condition.
Conservative therapy with antibiotics is the first-line treatment. At least 4 weeks of antibiotics is usually required, whereas patients with a hepatic abscess should receive at least 6 weeks of antibiotics [1] ; [3] . The choice of empiric antibiotics includes monotherapy with a carbapenem or a beta-lactam/beta-lactamase inhibitor, or combination therapy with metronidazole plus third-generation cephalosporins. The antibiotics should later be modified if culture results are available. Surgical intervention to remove the infection source may be indicated for infection control. Although recanalization with anticoagulation may be used to prevent intestinal ischemia, the role of anticoagulation is still controversial in septic thrombophlebitis [1] ; [3] .
Conflicts of interest
All authors disclose no conflicts of interest.
References
- [1] J.D. Rea, J.P. Jundt, R.L. Jamison; Pylephlebitis: keep it in your differential diagnosis; Am J Surg (2010), pp. e69–e71
- [2] R.M. Plemmons, D.P. Dooley, R.N. Longfield; Septic thrombophlebitis of the portal vein (pylephlebitis): diagnosis and management in the modern era; Clin Infect Dis, 21 (1995), pp. 1114–1120
- [3] Y.S. Chang, S.Y. Min, S.H. Joo, S.H. Lee; Septic thrombophlebitis of the porto-mesenteric veins as a complication of acute appendicitis; World J Gastroenterol, 14 (2008), pp. 4580–4582
- [4] C. Tait1, T. Baglin, H. Watson, M. Laffan, M. Makris, D. Perry, et al.; Guidelines on the investigation and management of venous thrombosis at unusual sites; Br J Haematol, 159 (2012), pp. 28–38
- [5] J.S. Levine, D.W. Branch, R. Rauch; The antiphospholipid syndrome; N Engl J Med, 346 (2002), pp. 752–763
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?