(Created page with "==Summary== ====Objectives==== In bilateral cleft lip/palate patients, sometimes the premaxilla is severely protruded and twisted. In such situations premaxillary osteotomy...") |
(No difference)
|
Revision as of 11:37, 26 May 2017
Summary
Objectives
In bilateral cleft lip/palate patients, sometimes the premaxilla is severely protruded and twisted. In such situations premaxillary osteotomy is beneficial. In this article a new technique for fixation of premaxilla after osteotomy is presented.
Methods
The lip-split approach and premaxillary osteotomy and ostectomy from bony nasal septum were carried out. Fixation of osteotomized premaxilla was achieved with low profile miniplate or microplate. Bone grafting of that side was performed during the same session.
Results
This procedure was performed in three patients, with good labial repair after the lip split. The bone graft was successful in all the three cases and there were no complication for premaxillary osteotomy in this series.
Conclusion
In protruding premaxilla, osteotomy and fixation of premaxilla with miniplate to the vomer bone during alveolar bone grafting through a lip-split approach yielded satisfactory results in patients requiring secondary functional cheilorhinoplasty.
Keywords
alveolar cleft bone grafting;Stabilization of premaxilla;internal fixation;premaxillary osteotomy
1. Introduction
In some bilateral cleft lip/palate patients the premaxilla is severely protruded and twisted; alveolar cleft becomes very wide and unmanageable. In such a situation, osteotomy of the premaxilla to set it back between lateral segments is useful.1
For fixation of osteotomized premaxilla some techniques and devices have been recommended, such as internal fixation with miniplate to fix it laterally to adjacent lateral segments, Kirshner wire that is inserted above and in between the maxillary central incisors and fixation of the premaxilla posteriorly, between the lateral segments and finally a cortical bone graft as a biologic plate that is secured to both sides of the cleft with a miniscrew.2 ; 3
Auxiliary devices such as occlusal splints and direct interdental wiring between the premaxillary central incisors and the teeth adjacent to the alveolar cleft margins are also beneficial.4 Cementing a bite splint, arch bar and orthodontic brackets can also be used for this purpose.
After premaxillary osteotomy fixation using routine methods, clinicians are commonly confronted with inadequate posteriorly positioned premaxilla, while it is not stable and has noticeable movements. Tipping of the premaxillary segment is the other problem. In this article, a new technique is presented for bodily movement and fixation of premaxilla after osteotomy. Although the miniplate has been applied for fixation of osteotomized premaxilla as described by Carlini et al,3 the technique we are presenting has several basic differences: the osteotomized premaxilla is fixed posterosuperiorly to the vomerian bone, not to the lateral segment, and there is no fear of damaging the teeth (erupted or unerupted) adjacent to the bony cleft margin. The greatest advantage of this technique is that it is actually ostectomy instead of osteotomy—a fact that prevents the tipping of the premaxillary segment. Fixation to the vomerian bone is also done with Kirshner wire, but the presented technique is more predictable and less technique-sensitive.
2. Methods and patients
2.1. Methods
Patients with bilateral cleft lip/palate who require osteotomy of the premaxillary segment, with bad lip scar from previous surgeries, were included into the study. Palatal constriction should be corrected prior to the surgery. The minimum age for premaxillary osteotomy was considered to be 8 years, to prevent possible interference with maxillary growth. Preoperative orthopantomograph and lateral cephalometry were taken in every case, and if more details were needed, then cone beam computer tomography was ordered.
This technique requires a lip-split approach to the nasal septum. The nasal septum was accessed through the previous lip scar, and then the mucoperiosteum over the premaxillary stalk is reflected. With a fissure bur in a high-speed straight surgical handpiece, a block of the bone is removed from this stalk. Considerable attention is given so as not to injure the mucosa of the nasal septum on the opposite side. The choice over left- or right-side bone grafting is first based on the size of the cleft and second by surgeon preference.
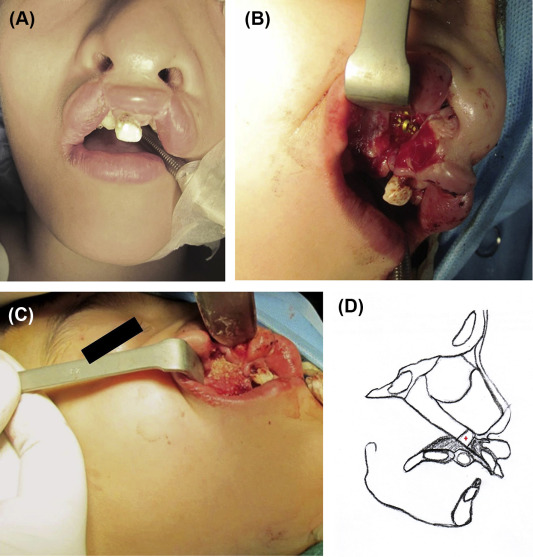
After osteotomy and ostectomy, the premaxilla is repositioned posteriorly and superiorly (if indicated) and internally fixed with a three-hole titanium miniplate. Based on the thickness of the bone, bicortical screws with appropriate length were used to secure the miniplates (1 screw in each segment). The amount of ostectomy was decided preoperatively by prediction tracing of lateral cephalometry. The reflected mucoperiosteum is sutured with 4–0 resorbable sutures, and in the same session alveolar bone grafting of this side is carried out. The side with the wider alveolar gap was chosen for bone grafting. The bone grafting on the other side is performed in a separate session 3 months later in the usual manner without the need for lip split (Figure 1).
|
|
|
Figure 1. (A) Protruded premaxilla and whistle lip deformity. (B) Lip split, setback of premaxilla, and internal fixation to bony nasal septum with a three-hole miniplate. (C) Ostectomy bone admixed with artificial bone substitutes for bone grafting. (D) Schematic picture. The plus symbol (+) points to the ostectomy block. |
2.2. Patients
2.2.1. Case 1
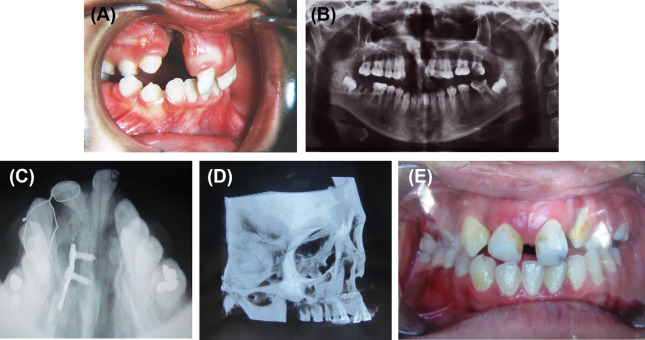
The patient was a 22-year-old girl with bilateral cleft lip/palate and protruded premaxilla. There was a large oronasal fistula posterior to the premaxillary segment. The lip had undergone surgery in infancy, but a severe whistle deformity and a visible muscle bulge at the lateral segments were evident. The premaxilla was set back using the above-mentioned procedure and the bone was grafted (unilaterally; Figure 2). Bone grafting on the other side was performed in a separate session. The patient was followed up for 4 years.
|
|
|
Figure 2. (A) Protruded premaxilla. (B) Orthopantomograph view showing rotated premaxilla. (C) Occlusal radiograph 3 months after the operation showing appropriate fixation and consolidation of bone graft in the right side. (D) Postoperative cone beam computer tomography (CBCT). (E) Postoperative photograph 3 months after the operation. |
2.2.2. Case 2
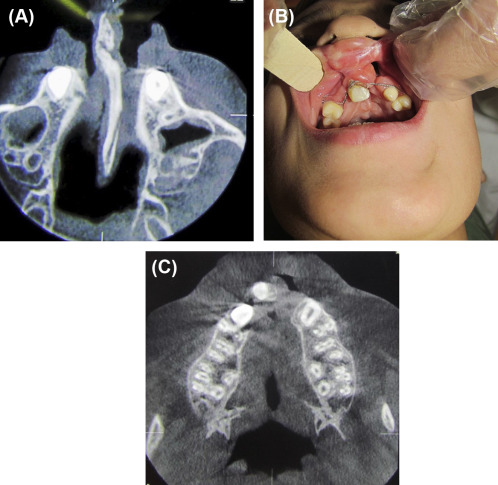
The patient was an 11-year-old boy with an unsuccessful previous operation for the closure of a bilateral alveolar cleft. The premaxilla was protruded and extruded. It was managed with this new technique (Figure 3). This patient was followed up for 2 years.
|
|
|
Figure 3. (A) Protruded premaxilla and thick bony septum. (B) Clinical result 1 month after the operation. Interdental wiring is used for further stabilization. The right side was bone grafted simultaneously with premaxillary osteotomy. (C) Cone beam computer tomography (CBCT), 3 months after the operation shows premaxilla, correctly aligned with lateral segments (one side bone grafting). |
2.2.3. Case 3
The patient was an 8-year-old boy with unsightly protruded premaxilla. He had experienced an unsuccessful tongue flap for the closure of a large palatal fistula. It was managed like the other two cases presented above (Figure 4). This patient was followed up for 1 year.
|
|
|
Figure 4. (A) Protruded premaxilla. (B) Cropped orthopantomograph (OPG) after premaxillary osteotomy and bone grafting. |
3. Results
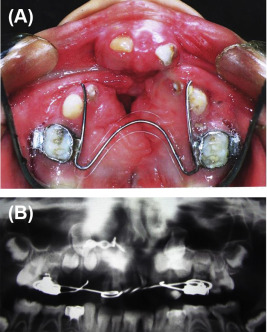
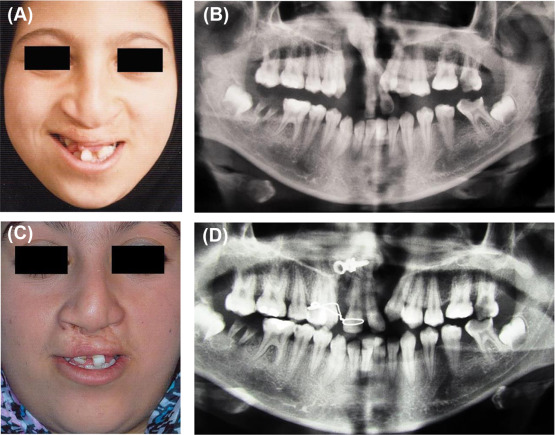
This procedure was performed in three patients, with good labial repair after the lip split. The bone graft was successful in all cases, and there was no complication for premaxillary osteotomy in this series. The premaxilla was stable and firmly adhered to the lateral segments with bone (Figure 5).
|
|
|
Figure 5. (A) Photograph taken during childhood shows protruded and twisted premaxilla. (B) Orthopantomograph (OPG) prior to the surgery. (C) Full-face photograph taken 3 months after the first surgery. Note the healed right lip scar and improvement in lip shape. The left side bone grafting was performed using the conventional method. (D) OPG taken 3 months after the premaxillary osteotomy and right side bone grafting. |
4. Discussion
Osteotomy of the premaxilla is not a routine procedure if orthodontic and orthopedic treatments on bilateral cleft lip/palate patients are applied at the right time. Occasionally, surgeons encounter cleft patients with protruded premaxilla and neglected alveolar cleft. In such situations, premaxillary osteotomy is beneficial.
Historical lessons gleaned from this topic reveal that total and subtotal premaxillectomy and premaxillary osteotomy during lip closure have bad effects on further facial growth; therefore, these procedures are postponed nowadays.5 ; 6
Osteotomy of the premaxilla at the time of alveolar cleft bone grafting is an acceptable procedure.7 Current complication of premaxillary osteotomy results from inadequate fixation that prevents bony union and leads to mobile premaxilla.8 Tipping of the premaxillary segment resulting from an inadequate premaxillary stalk bone removal (osteotomy instead of ostectomy) is a common problem. This is attributed to the limited access to the region through incisions on and lateral to the premaxilla and endonasal premaxillary osteotomies.9 ; 10 In patients with wide residual palatal clefts, good exposure of the vomer is possible, so tipping of premaxilla after osteotomy/ostectomy is not a problem.11
The presented technique internally fixes the osteotomized segment and bodily moves the premaxilla in the posterior direction. The lip split gives wide access not only for removing bone from the solitary midline septal/vomer bony connection of the premaxilla to the midface but also provides wide access to the nasal floor and makes it easier to repair the nasal floor. This technique is not indicated for every bilateral cleft patient with protruded premaxilla. If the patient presents with normal shape of the lip but with protruding premaxilla, then this technique is not suitable.
All patients required interdental wiring for stabilization, because one plate fixation is not rigid enough. However, the presented technique can help control the osteotomized premaxilla three-dimensionally. Bodily movement of the osteotomized premaxilla and doing the procedure without fear of injury to the unerupted or erupted teeth are the other advantages of this technique.
Alveolar cleft bone grafting adds stability and vascularity to the repositioned premaxilla after bridging these two segments.12; 13; 14 ; 15 In our patients, the side accessed by lip split was bone-grafted during the first session, and the other side was repaired in a separate procedure as recommended by Akita and Hirano.16 However, bilateral bone grafting in one session has also been recommended.17 ; 18 We preferred two-session surgeries, because it was our first experience in using this technique. In the next cases, we will try to use both side alveolar bone grafting and premaxillary repositioning simultaneously in a single procedure.
Use of resorbable plates can be a good alternative to titanium miniplates, as it omits the need for answering the question “If permanent titanium implants were used, were they removed, and how soon after the first surgery?” We used titanium miniplate, and there was no need to remove it in the three cases presented in this article, but if the surgeon is inclined to remove the titanium miniplate, the recommended time is during the second surgery for alveolar bone grafting of the other side.
The presented technique is recommended during alveolar cleft bone grafting in cases with severely protruded premaxilla that require secondary functional cheilorhinoplasty for improving residual lip and nasal deformities. There should be a thick vomerian bone in connection to the premaxilla on preoperative occlusal radiographs,19 ; 20 and the collapsed maxillary arch should be expanded prior to the surgery. A repositioned premaxilla reduces the size of palatal fistulas and eliminates the need for tongue flaps to close this type of fistulas.
5. Conclusion
In protruding premaxilla, osteotomy and fixation of premaxilla with a miniplate to the vomer bone during alveolar bone grafting through lip-split approach has satisfactory outcomes in patients who require secondary functional cheilorhinoplasty.
Acknowledgments
This study was supported by a grant from the Vice Chancellor of Research of Mashhad University of Medical Sciences, Mashhad, Iran.
References
- 1 J.K. Scott, R.M. Webb, T.R. Flood; Premaxillary osteotomy and guided tissue regeneration in secondary bone grafting in children with bilateral cleft lip and palate; Cleft Palate Craniofac J, 44 (2007), pp. 469–475
- 2 J.C. Posnick, B. Tompson; Modification of the maxillary Le Fort I osteotomy in cleft-orthognathic surgery: the unilateral cleft lip and palate deformity; J Oral Maxillofac Surg, 50 (1992), pp. 666–675 discussion 75–76
- 3 J.L. Carlini, C. Biron, K.U. Gomes, R.M. Da Silva; Surgical repositioning of the premaxilla with bone graft in 50 bilateral cleft lip and palate patients; J Oral Maxillofac Surg, 67 (2009), pp. 760–766
- 4 P. Batra, V. Agrawal, H.J. Kiran, S.B. Madanagowda; Treatment of a patient with a bilateral cleft lip and palate with implants and surgery of the maxillary anterior region; World J Orthod, 11 (2010), pp. 380–386
- 5 M.N. Saad, D.I. Smith, C.T. Khoo; Subtotal premaxillectomy; a salvage procedure in selected cases of bilateral cleft lip and palate; Br J Plast Surg, 40 (1987), pp. 396–406
- 6 B.L. Padwa, A. Sonis, S. Bagheri, J.B. Mulliken; Children with repaired bilateral cleft lip/palate: effect of age at premaxillary osteotomy on facial growth; Plast Reconstr Surg, 104 (1999), pp. 1261–1269
- 7 T. Bartzela, C. Katsaros, E. Ronning, et al.; A longitudinal three-center study of craniofacial morphology at 6 and 12 years of age in patients with complete bilateral cleft lip and palate; Clin Oral Investig, 16 (2012), pp. 1313–1324
- 8 H. Aburezq, J. Daskalogiannakis, C. Forrest; Management of the prominent premaxilla in bilateral cleft lip and palate; Cleft Palate Craniofac J, 43 (2006), pp. 92–95
- 9 B.L. Eppley, A. Sclaroff, J.J. Delfino; Secondary management of the premaxilla in bilateral cleft lip and palate patients; J Oral Maxillofac Surg, 44 (1986), pp. 987–998
- 10 R.C. Mixter, G. Stroncek, J. Doyle, L. Carson; Endonasal premaxillary osteotomy; Plast Reconstr Surg, 97 (1996), pp. 1494–1496
- 11 R.K. Narayanan, S.A. Hussain, S. Murukesan, J. Murthy; Synchronous palatal closure and premaxillary setback in older children with bilateral complete cleft of lip and palate; Plast Reconstr Surg, 117 (2006), pp. 527–531
- 12 S. Sindet-Pedersen, H. Enemark; Comparative study of secondary and late secondary bone-grafting in patients with residual cleft defects. Short-term evaluation; Int J Oral Surg, 14 (1985), pp. 389–398
- 13 G. Paulin, P. Astrand, J.B. Rosenquist, L. Bartholdson; Intermediate bone grafting of alveolar clefts; J Craniomaxillofac Surg, 16 (1988), pp. 2–7
- 14 N. Amanat, J.D. Langdon; Secondary alveolar bone grafting in clefts of the lip and palate; J Craniomaxillofac Surg, 19 (1991), pp. 7–14
- 15 A. Rahpeyma, S. Khajehahmadi; Modified VIP-CT flap in late maxillary alveolar cleft surgery; J Craniomaxillofac Surg, 42 (2014), pp. 432–437
- 16 S. Akita, A. Hirano; Usefulness of simultaneous pre-maxillary osteotomy and bone grafting in the bilateral clefts; J Craniofac Surg, 17 (2006), pp. 291–296
- 17 M.J. Kim, J.H. Lee, J.Y. Choi, N. Kang, J.H. Lee, W.J. Choi; Two-stage reconstruction of bilateral alveolar cleft using Y-shaped anterior-based tongue flap and iliac bone graft; Cleft Plate Craniofac J, 38 (2001), pp. 432–437
- 18 Y.L. Jia, D.R. James, M. Mars; Bilateral alveolar bone grafting: a report of 55 consecutively-treated patients; Eur J Orthod, 20 (1998), pp. 299–307
- 19 K. Smolka, N. Eggernsperger, T. Iizuka, W. Smolka; Evaluation of secondary functional cheilorhinoplasty during growth of cleft patients with residual lip and nasal deformities; J Oral Maxillofac Surg, 66 (2008), pp. 2577–2584
- 20 H.P. Freihofer, P.A. van Damme, A.M. Kuijpers-Jagtman; Early secondary osteotomy-stabilization of the premaxilla in bilateral clefts; J Craniomaxillofac Surg, 19 (1991), pp. 2–6
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?