Highlights
- Research shows that addiction is typically a limited not chronic disorder.
- Most addicts reduce drug use voluntarily.
- Smokers and heroin addicts can regulate their cravings as a function of drug availability.
- According to testable definitions of voluntary behavior and free-will, addicts have both.
Abstract
Introduction
This paper addresses two overlapping questions: Do addicts have the capacity to voluntarily quit drugs? And do individuals knowingly pursue courses of action that they realize are bad for them, such as excessive drug use?
Methods
I propose two testable versions of free will. First, the observation that activities differ in the degree to which they are susceptible to the influence of their consequences (e.g., costs and benefits) has proven a useful criterion for classifying behavior as voluntary or involuntary. Thus, we can ask if drug use in addicts is influenced by its consequences. For instance, do laws that promise legal sanctions for drug use reduce drug use in addicts? Second, the philosopher Harry Frankfurt proposed a definition of free will that takes into account desires and self-reflection. I propose that addicts who do not want to desire drugs and successfully stop craving drugs pass his test.
Results
Dependence on illicit drugs typically ends after about four to six years. Dependence on cigarettes and alcohol persists for much longer, but most smokers and alcoholics eventually voluntarily quit using. Smokers and heroin addicts can voluntarily regulate their drug cravings as a function of the availability of their drug of choice. They have the capacity to pass Frankfurts test of free will.
Conclusions
Addicts have free will as defined by the capacity to voluntary quit using drugs and to voluntarily regulate their cravings.
Keywords
Addiction;Substance dependence;Free will;Choice;Drug craving;Compulsion
1. Introduction
Socrates claimed that individuals could not knowingly embark on a course of action that they thought unwise or bad: “No one goes willingly toward the bad.” If we apply this idea to drug use, then we should expect that no one would relapse who had quit after careful consideration of the costs and benefits of shooting heroin or smoking crack. However, addicts do relapse. Assuming Socrates is correct then drug use must not really be an instance of what one “willingly” goes “toward;” it must be compulsive. That is, even if addicts want to abstain, they can't. This line of reasoning is not new. More than four hundred years ago in what is likely one of the earliest recorded discussions of alcoholism, British clergy labeled alcoholism a “disease” that robbed its victims of “all rules of reason” and was “so epidemical” that “all the physicians in England know not how to stop it.” (See Jessica Warners paper (1994) for the original text and her discussion of addiction as a pre-industrial age concept.) Today, addiction experts, science journalists, and the informed public make the same claims, although they have a much more detailed and powerful data base for doing so than did 17th century clergymen. Anatomical investigations offer detailed pictures of drug-altered nervous tissue (Robinson, Gorny, Mitton, & Kolb, 2001), brain imaging studies reveal correlations between drug use and brain anatomy and function (Wang et al., 2016), and familial studies reveal genetic correlates of addiction (Palmer et al., 2015).
Nevertheless, the question of whether addicts are compulsive drug users remains controversial. In a series of recent publications, clinicians, neuroscientists, and philosophers have simply assumed or explicitly made the argument that addicts remain voluntary drug users (Ainslie, 2013; Hart, 2013; Higgins et al., 2000 ; Sinnott-Armstrong and Pickard, 2013). Research on the biology of drug use and addiction is well known, yet the argument that addicts retain the capacity to say “no” to drugs has, if anything, gained more adherents in recent years (Heather and Segal, 2016 ; Lewis, 2015). Thus, it is fair to say that today there are two versions of addiction. In the statements of the federal health agencies that support addiction research and in countless journal articles, particularly those by neuroscientists, the reader is greeted by the phrases “addiction is a chronic relapsing disease” and “compulsive drug use,” along with the implication or explicit claim that addicts want to stop using, but, against their will, get high anyway. In contrast, in many of the papers that focus on patterns of drug use, the key phrases are “voluntary,” “choice,” “alternatives” and “contingencies.” Much is at stake. How addiction is classified is critical for strategies on how to best reduce the harm it causes, health policy, and what people who use drugs in excessive amounts expect of themselves.
In what follows, I test two understandings of free will as they apply to individuals who meet the American Psychiatric Association criteria for “substance dependence” (the APAs term for addiction, e.g., DSM-IV, 1994). One is based on how the term has been used in addiction research; the other is based on the philosopher Frankfurts (1971) discussion of what it means to be a person. In addiction research, free will is synonymous with voluntary behavior. Hence, I test the proposition that addicts can voluntarily quit using drugs. Frankfurts account takes into consideration the role that self-reflection might play in regard to desires and the attempt to regulate ones desires. For example, imagine an addict who says to him or herself: “I do not want to desire drugs.” As a way of empirically testing whether this might occur or could occur, I test whether smokers regulate their cravings for cigarettes and whether heroin addicts regulate their cravings for heroin. Thus, the goal is to put widely assumed and/or discussed ideas about the nature of voluntary behavior and free will into testable forms and evaluate whether addicts have free will.
2. How to tell voluntary and involuntary behavior apart
In her blog on the National Institute on Drug Abuse (NIDA) website, Nora Volkow, the institutes current director, wrote that the slogan “addiction is a brain disease” was not specific enough; in its place, she substituted “drugs rob the brain of the capacity to exercise free will" (https://www.drugabuse.gov/about-nida/noras-blog/2015/06/addiction-disease-free-will). Her predecessor, Alan Leshner, made a similar claim (1997). In an article published in Science, he stated that addicts start off as voluntary drug users but then as a function of drug use itself, he or she is turned into a compulsive, involuntary drug user (exactly what early 17th century clergy claimed). However, neither Volkow nor Leshner offer testable definitions of what they mean by free will, the loss of free will, or involuntary behavior. For instance, Volkow does not define any terms but instead recounts a moving anecdote about her grandfather who was an alcoholic. He kept drinking even though he was painfully aware of the harm he was bringing upon himself and his family. Given her conclusion that her grandfather had lost the ability to exercise his will, what she must have in mind is that self-destructive behavior is prima facie evidence of the loss of free will. Indeed, she presents no other evidence. In effect, the story is an example of Socratess claim that no one can act against their own best interests, with the qualifier: unless they have a disease of the will, as can be caused by alcohol or other addictive drugs.
However, the idea that self-destructive behavior is necessarily a sign of compulsion is not credible. For instance, voluntary yet self-destructive acts drive the plot line of many (perhaps most) novels, plays, and movies. Agamemnon exchanged the life of his daughter for the promise that his ships would safely leave port and more speedily carry out the plan to sack Troy. But once underway, he undermined his own plans by demanding that Achilles, his greatest warrior, turn over his loveliest female slave. As could only be expected, Achilles, furious at Agamemnon, pulls his troops from the war. In both instances, Agamemnon acted selfishly and, in doing so, caused and/or risked great harm to himself and others.
Although the Iliad dates from about the 8th century BC, the story remains fresh. Bill Clinton repeatedly risked his reputation for the sake of illicit dalliances and eventually sabotaged his presidency, and the chances of his vice-president to succeed him, for a fleeting affair with a naïve White House staffer. Agamemnon and Bill Clinton were not dysfunctional men; they were proven leaders, who, under most circumstances, made winning choices. If asked, “How should one rule?” Agamemnon would have recommended ensuring the loyalty of ones best soldiers, just as Bill Clinton would have recommended prudence in personal conduct. Agamemnon and Clintons stories are dramatic, because of what was at stake. However, the manner of their actions was commonplace: Goaded by their immediate concerns, Agamemnon and Clinton heedlessly ignored the advice of others and, likely, the advice that they themselves would have given others. Then, when the costs of their actions began to take hold, they repented. In short, self-destructive behavior does not necessarily imply compulsion. Whether or not addicts are involuntary drug users is an empirical question, one that requires measurable definitions of the key terms.
2.1. Two versions of “free will”
In what follows, I test two versions of free will. One is typical of how addiction researchers have discussed the topic; the other is representative of how philosophers have discussed the topic. The addiction version is synonymous with voluntary behavior, which is something that all animals exhibit, as described below. The philosophers version is defined in ways that makes it specific to humans. Consequently, it seems more fitting to refer to the addiction researchers version as “voluntary behavior.”
2.2. Activities differ in susceptibility to their consequences
Behavior is purposive. However, activities vary in terms of the nature of the causal relations that link behavior to its goals. Consider some familiar examples: winks vs. blinks, applying rouge, vs. blushing, spitting vs. sneezing, and kicking a ball vs. the patellar reflex. Whether we wink, apply cosmetics, or kick a ball depends on the costs and benefits associated with these acts. For instance, the soccer player kicks or fakes a kick to advance his teams chances of winning and learns to be more effective at doing so as a function of feedback in the form of successes and failures. In contrast, blinks, blushing, and the patellar reflex are driven by stimuli. Once in motion, they proceed, even if doing so fails to achieve a desired aim. Experience appears to play little or no role in the perfection of blinking. Indeed, the simplest elicited reflexes are wired so that they can take place without input from the brain. William James summarized these ideas in an apt comparison of Shakespeares Romeo and iron filings (2013/1890). James points out that the iron filings are as attracted to a magnet as Romeo is to Juliet, but construct a barrier and Romeo will find a way around it; he will learn to adjust his behavior according to the consequences of his efforts. In contrast, the iron filings continue to press “stupidly” forward, never deviating from their path regardless of their lack of progress.
In the lab the distinctions outlined above are typically described in terms of two contrasting causal relations. Winks, kicks, making oneself attractive, and romantic relations are under the control of feedback, as in reinforcement learning studies. Blinks, blushing, and instincts are under the control of eliciting stimuli. They are triggered, just as a WW II rocket once let loose cannot change its course, even when its target has taken evasive actions. We say activities are “voluntary” when they are controlled primarily by their consequences, and we say “involuntary” when the activity is largely under the control of eliciting stimuli. Thus, the distinction is not between causality and its absence, but between types of causality.
2.2.1. Social manifestations of the distinction between voluntary and involuntary behavior
Although the examples are everyday activities, they are important. Social practices and social policy vary markedly as a function of whether the behaviors of interest are voluntary or involuntary. During flu season, office workers are asked to wash their hands as often as possible, but no one is asked not to sneeze. In the courts, the type and degree of punishment varies as a function of the degree to which the criminal act was judged to be voluntary. In science, disciplines organize themselves as dictated by the distinction between voluntary and involuntary. Psychologists tend to study voluntary learned behavior, whereas biologists and ethologists tend to study elicited behavior. In settings in which behavior matters, a critical concern is the degree to which the behaviors in question are voluntary.
2.2.2. The voluntary/involuntary continuum: A matter of degree
The labels “voluntary” and “involuntary” suggest mutually exclusive, binary categories. However, even the simplest activities include both eliciting triggers and feedback-enabled consequences. Two examples help make the point. In a paper aptly called How an Instinct is Learned, Hailman (1969) describes the development of feeding in laughing gull chicks as a “mosaic” composed of learned and unlearned components that cannot be meaningfully separated. Naïve chicks clumsily peck at any gull-like head and have no innate appreciation of the differences between food bits and non-food bits. But, as a function of successful feeding, they learn to discriminate food from non-food and skillfully beg food from their parents. Similarly, laboratory behavioral research reveals evolutionary constraints that bias what is learned and how easily it is learned. Rats more readily learn to associate taste with sickness and a bell with shock. The implication of these cases for the understanding of the distinction between voluntary and involuntary behavior is that we should expect borderline cases that are difficult to classify and that some activities will be voluntary in one context but not another. Tourettes syndrome provides an instructive example of context-dependent changes in voluntariness.
Oliver Sacks, the neurologist and author, described a physician with Tourettes syndrome who did not tic when he was piloting an airplane or in surgery (1995). In the film documentary Twitch and Shout, we meet a cabaret singer with Tourettes syndrome who does not tic when she is singing ( Chiten, Medley, & Russel, 1994). However, most would agree that it would be incorrect to say that these cases show that Touretters tic voluntarily. Rather, the cases show that under extraordinary conditions, some Touretters can predictably control their tics. But, by definition we do not expect people to be extraordinary. Thus, it is reasonable to classify Tourettes syndrome as an involuntary disorder. Assuming that addicts can control their drug use at least some of the time, we will want to know if this occurs only under extraordinary circumstances or if it can occur in response to everyday concerns and pressures.
Although this is a bare bones account of the differences between voluntary and involuntary behavior, it is sufficiently detailed to generate explicit testable predictions of whether addicts are voluntary or involuntary drug users.
3. The logic of voluntary behavior and its implications for addiction
The definitions of voluntary and involuntary behavior introduced in the previous section yield explicit testable predictions for the natural history of addiction. Consider first the implications of the claim that addicts remain voluntary drug users.
3.1. What to expect if addicts remain voluntary drug users
According to the idea that voluntary actions vary as a function of their consequences, then the benefits of voluntary drug use must outweigh its costs. But the label “addiction” identifies a pattern of drug use in which the consequences are, on balance, negative. Otherwise, addiction would not be considered a disorder; otherwise, getting drunk or high on a daily basis is self-medication; otherwise, clinicians and researchers are mislabeling self-medication a disease. Thus, if drug use remains voluntary, it is reasonable to expect that disordered, addictive drug use should not emerge, or, if it does, then it should not persist for long.
3.2. The costs and benefits of drug use change over time
The logic is correct but ignores temporal changes in the costs and benefits of drug use and the possibility of an extended period in which the costs and benefits more or less balance each other out.
The consequences of drug use change over time. Initially, there is a “honeymoon” period in which few, if any, of the costs have time to emerge. But, as drug use continues and becomes more frequent, the consequences begin to include direct negative effects, such as tolerance and withdrawal, and indirect, socially mediated penalties, such as criticism from friends, legal problems, financial problems, workplace problems, and the like. Over time, the negative effects accumulate and the positive effects fade (e.g., tolerance) so that eventually the costs outweigh the benefits. Thus, if addicts remain voluntary drug users, they should eventually quit. Moreover, since voluntary behavior is maintained by feedback, it is both self-sustaining and self-attenuating. Applied to drug use, this means that it should be possible for addicts to quit drugs without professional assistance. This does not mean that professional assistance is of no value. Quitting is always difficult if not excruciating (as outlined in Sections 6 and 7), and we routinely employ teachers and coaches when voluntary activities are challenging. These predictions could not be more at odds with received wisdom regarding the nature of addiction and, thus, should be easy to test (and presumably easy to disprove).
3.3. What to expect if addicts are involuntary drug users
If addicts are involuntary drug users who cannot quit because they no longer have the will power to do so, then an outside intervention is prerequisite for any chance of recovery. In line with this logic, those who claim that addiction is a disease, such as the directors and spokespersons for the federal health bureaucracies, put much of their resources into the search for pharmacological cures. Since no clearly effective addiction medicines have yet to appear, the backup plan is intensive long-term clinical support. Charles O'Brien, director of University of Pennsylvanias Center for Studies of Addiction, and A. Thomas McLellan, a former Deputy Director of the Office of National Drug Control Policy, write that “[a]ddictive disorders should be considered in the category with other disorders that require long-term or lifelong treatment” (1996). A few years later they add: “… [the] effects of drug dependence treatment are optimized when patients remain in continuing care and monitoring without limits or restrictions on the number of days or visits covered” (2000). This is quite logical: if addiction is a disease and there is no cure then lifelong monitoring is in order.
Thus, the definitions of voluntary behavior and addiction combine to lead to clear and starkly different predictions regarding the natural history of addiction. If drug use remains voluntary, addicts should quit and can do so without professional help. If drug use becomes involuntary, then addiction is a chronic disorder that requires continuous professional care until a cure is found.
4. Quit rates
Which view is correct? Addiction clinic follow-up studies typically report that treatment was unsuccessful at securing abstinence, or, if an addict managed to stop using, it proved temporary (Gossop et al., 2003 ; Wasserman et al., 1998). However, most addicts do not seek treatment (Anthony and Helzer, 1991; Robins, 1993 ; Stinson et al., 2005), and those that do are much more likely to suffer from additional psychiatric and non-psychiatric disorders than addicts who stay away from the clinics (Regier et al., 1990 ; Rounsaville et al., 1991). Thus, it is possible that the clinic studies provide a distorted view of the natural history of addiction. Indeed, because of this problem, the US federal health institutes initiated a series of nation-wide surveys of the prevalence and correlates of psychiatric disorders in the general public. The surveys selected subjects so as to create a study population that was representative of the country as a whole, not just those in treatment. Having received treatment did not exclude anyone, but it was not a necessary requirement for being a participant. Thus, the results are more likely to provide a true picture of a disorders natural history than research based exclusively on either treatment or non-treatment populations. For instance, imagine that our understanding of the flu was based solely on those cases that ended up in the hospital (which is not to suggest that addiction is like the flu).
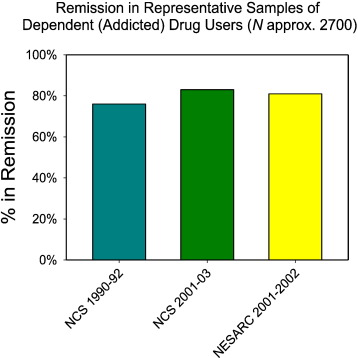
Fig. 1 shows the results for addiction for the three national studies that distinguished between abuse and dependence (Conway et al., 2006; Kessler et al., 2005; Stinson et al., 2005 ; Warner et al., 1995). Each project recruited thousands of subjects, with the most recent one, the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), topping the list at approximately 43,000. Pooling across the three studies, about 2700 participants met the DSM criteria for addiction to an illicit drug. On the x-axis are the three studies, along with the years in which the research was conducted. On the y-axis is the proportion of those who met the criteria for lifetime dependence on an illicit drug, but did not meet these same criteria for at least a year prior to the diagnostic interview. The graph shows that most addicts were ex-addicts. As the average age in these studies was about 42, the graph suggests that for most addicts dependence ends in their late twenties or early thirties.
|
|
|
Fig. 1. The percentage of individuals with a lifetime diagnosis of dependence on an illicit drug who did not meet the criteria for dependence for at least a year prior to the diagnostic interview in the three major US psychiatric surveys that distinguished between drug dependence and drug abuse. The dates indicate the period in which the research was conducted. |
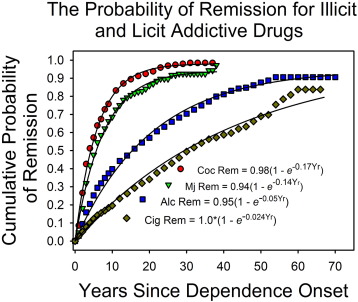
Fig. 2 confirms this inference. It shows the likelihood of remission, as a function of years since the onset of dependence for two illicit and two licit addictive drugs (Lopez-Quintero et al., 2011). On the x-axis is years since the onset of dependence. On the y-axis is remission. The smooth curves are the best-fitting exponential functions. The multiplier (e.g., 0.98 for cocaine) estimates the eventual likelihood of remission for all those who were ever dependent (the curve asymptote); the exponent estimates the average likelihood of remission each year.
|
|
|
Fig. 2. The cumulative probability of remission as a function of time since the onset of dependence, based on Lopez-Quintero et al.s (2011) report. The smooth curves are the best fitting exponential functions. The proportion of addicts who quit each year was approximately constant. The exponent in the equation estimates the constant quit rate. The multiplier estimates the asymptotic level of quitting. It was 0.94 and higher. The rate of quitting varied as a function of drug and drug availability. |
The asymptotic “recovery” levels exceeded 90%. As the model fits the data quite well, it is reasonable to assume that most drug users who meet the APA criteria for addiction will eventually recover. The exponents varied as a function of type of drug. However, the pattern appears to reflect drug availability rather than pharmacological factors. For instance, dependence was much more persistent for legal than for illegal drugs, and within each category, the more available drug was the one for which dependence lasted longer. That an exponential curve fits the data says that each year an approximately constant proportion of those still addicted went into remission regardless of how long they have been dependent. As discussed elsewhere, this is a surprising result (Heyman, 2013 ; Heyman and Mims, 2016).
Although Fig. 2 says that the conditional probability that dependence ends was approximately constant, there was considerable individual variation as to when this happened. For instance, dependence persisted for four years or less for about half of those with a lifetime diagnosis of cocaine dependence. Yet, a quarter of those dependent on cocaine remained heavy users for 10 years or more, and 10% were dependent on cocaine for 15 years or more.
Recall that the logic of voluntary behavior says that it should be possible for dependence to end without explicit, targeted interventions. In support of this prediction, addiction researchers report that most of those who meet the APA criteria for addiction do not make use of clinical services (Stinson et al., 2005, and see Anthony and Helzer, 1991 ; Robins, 1993). This of course does not mean that clinical interventions may not function as a useful catalyst. Rather the point is that the idea that addicts remain voluntary drug users predicts the high recovery rates and the manner in which recovery took place.
4.1. Are the national survey addiction results reliable?
Given that these results are so at odds with widely-held understandings of addiction, it is reasonable to assume that the national epidemiological surveys are seriously flawed. Possible methodological shortcomings are deceptive subjects, failures of memory, and differential cooperation. Perhaps those who were more likely to cooperate with the researchers were also more likely to remit. These and related concerns have been discussed in some detail elsewhere (Colón et al., 2002; Darke, 1998; Heyman, 2013 ; Weatherby et al., 1994). The consensus is that the epidemiological studies are not misleading. (1) The survey researchers go to great lengths to guarantee the participants' anonymity, and studies which combine metabolic tests of drug use with measures of self-reported drug use find that drug users are truthful when they have no strong reasons to fear negative consequences (Colón et al., 2002; Darke, 1998 ; Ledgerwood et al., 2008). (2) In support of these results, logic and calculations indicate that bias in recruiting subjects cannot explain the high remission rates. For example, it is possible to estimate the number of persons addicted to illicit drugs who would have had to be missing in order to reverse the obtained results. For example, if we assume that about 80% of those who ever became addicted were still addicted at about age 45, there would have to be approximately 20 million missing addicts that no one knew about (calculations in Heyman (2013)). This is not plausible. (3) The results displayed in Fig. 1 ; Fig. 2 have been replicated by studies that recruited subjects independent of treatment history but otherwise used quite different methods. For instance, in two studies in which there was repeated face-to-face contact with the subjects and access to information that allowed the researchers to validate drug use, including urine tests, remission rates were closer to 100% than to 50% (Robins, 1993 ; Robins and Murphy, 1967). Thus, it seems unlikely that methodological shortcoming explain the high remission rates of Fig. 1 ; Fig. 2.
4.2. The correlates of quitting drugs
Fig. 1 ; Fig. 2 say nothing explicit about how dependence comes to an end. However, that most of those who meet the DSM criteria for drug dependence did not seek treatment suggests that quitting was in response to the pressures of everyday life. That is, in the absence of an explicit intervention, changes in drug use must be a function of everyday circumstances. Two quite different literatures support this inference: studies of non-clinic drug users (Biernacki, 1986; Toneatto et al., 1999 ; Waldorf et al., 1991) and studies of the effects of nation-wide changes in government policies regarding drug use.
Research on non-clinic drug users relies largely on extended interviews and questionnaires. These reports provide a transcript of what addicts say about quitting. Among the themes that get the most emphasis are (1) the conflict between continued drug use and practical concerns and (2) the ethical implications of drug use. The following paraphrased quotes are typical: “I wasn't raised to be a bad parent,” “I wanted my parents to be proud of me,” “I was too old to go back to jail,” “I could no longer afford drugs and groceries,” “I knew I would die if I didn't stop,” “I wasn't born in order to become a drug addict.” However, these concerns cannot be the whole story. Prior to quitting, these same pressures were in force, but drug use continued. This suggests that a threshold was reached or there were psychological changes that made heavy drug use no longer bearable.
The self-report literature is buttressed by the historical record. The events have many of the properties of an experiment. There is a marked change in one or more critical conditions and a public record of what followed. However, unlike a lab experiment, we do not have to guess as to how the results might apply to drug use outside of the lab. The historical events include the Harrison Narcotics Tax Act of 1914, which criminalized the non-medical use of opiates and cocaine, Prohibition (1920–1933), which restricted the sale of alcohol, and the 1964 Surgeon Generals report on the health risks of cigarette smoking.
According to historians and reports from the 1920s, the Harrison Act reduced opiate use and addiction, perhaps by as much as 50% (Courtwright, 1982 ; Kolb and DuMez, 1981/1924). The Volstead Act was followed by a marked increase in the price of alcohol and a concomitant decrease in alcoholism (at least at first), as indexed by an abrupt decrease in the rate of cirrhosis of the liver (Miron and Zwiebel, 1991 ; Seeley, 1960). The 1964 Surgeon Generals report on the health risks of smoking was followed virtually immediately by a steady, approximately linear decrease in the prevalence of smoking, despite the fact that most smokers were pack-a-day addicted smokers (U.S. Department of Health and Human Services, 1990 ; U.S. Department of Health and Human Services, 1994). The historical trends are exactly as expected if addicts retain the capacity to quit drugs. In contrast, new laws, increases in prices, and newly published scientific information do not slow down the growth of cancer cells, improve memory in Alzheimers patients, or restore a receptors affinity for insulin.
4.3. Summary: Data support logic of voluntary behavior
The logic of voluntary behavior predicts that dependence is a limited disorder and that addicts can quit voluntarily. This is exactly what the data show. When researchers select drug users independently of their treatment history, addiction typically comes to an end in early or mid-adulthood. The conditions linked to the end of drug dependence are those that are central to well-being: family, job, and freedom. In addition, ex-addicts often stress values such as wanting to be a positive, helpful person. These are the conditions and goals that play a role in the business of life for most people; they are critically important but not extraordinary. Treatment studies often tell a different story. In many, perhaps most, the majority of addicts relapse. However, some programs are quite successful (see, e.g., Davis et al., 2016), and for those which repeatedly tracked their graduates, recovery levels increased at each evaluation (see Heyman, 2013). The different outcomes reflect higher comorbidity rates for clinic drug users, and likely other differences as well. Unfortunately, the differences between treatment seeking and non-treatment seeking addicts have not received the attention that they deserve.
5. Free will as the regulation of drug cravings
According to the definition of voluntary as susceptibility to the influence of consequences then Fig. 1 ; Fig. 2 and the attendant discussion show that addicts are voluntary drug users. These results also meet the understanding of free will that backers of the disease model have in mind when they assume that not quitting implies compulsion. However, according to many of the philosophers who write about free will, there is more to the issue than susceptibility to consequences. For instance, (1) all animals are capable of learning, (2) learning is behavior shaped by its consequences, (3) yet those who grant free will to humans are not likely to also grant it to all the species capable of learning. For instance, bees are capable of many of the types of learning observed in humans (e.g., Perry, Barron, & Cheng, 2013), yet it seems incongruous to say that bees have free will. Harry Frankfurt introduced a theory of free will that includes the relationship between self-reflection and action, a step which greatly reduces who qualifies for free will.
5.1. Harry Frankfurts approach to free will
Frankfurt begins by pointing out that animals have motives and make choices, but only humans evaluate their motives and choices. For example, consider a young man who is temperamentally shy but wants to be more outgoing and unafraid of shining the spotlight on himself. In Frankfurts analysis, temperamentally avoiding attention is a first-order desire, whereas not wanting to be a person who avoids attention is a second-order desire. A second-order desire that leads to effective action is a second-order volition: for example, the temperamentally shy person who wants to stop being shy and succeeds in altering his temperament. According to Frankfurt, someone chooses freely when his or her first-order and second-order desires coincide. For instance, a willingly shy person (one satisfied with being a shy person) has free will, as does the person who does not want to be a shy person and learns to not feel self-conscious in social settings. We can apply these ideas to addiction, although in a way that Frankfurt did not consider. He assumed that addicts did not have the capacity to become ex-addicts, so that the only choice for an addict was to be a willing or an unwilling addict. (Frankfurt discussed addiction well before the data reviewed in Fig. 1 ; Fig. 2 were available.) For a nuanced account of Frankfurts ideas as they relate to addiction, see Pickard (2017).
According to my adaptation of Frankfurts analysis, one of the ways that an addict can have free will is to (1) disapprove of himself as a person who desires drugs over non-drug alternatives, and then to (2) regulate his desire for drugs so that they are no longer paramount. Research on drug craving provides experiments that test whether this sequence of events is possible in the following sense: Can addicts regulate their craving for drugs, in particular, by reducing them when it is beneficial to do so? That is, just as addicts can quit using drugs, can they also alter their desires for drugs so that they are more in line with the sort of person they want to be?
5.2. Drug craving
The introduction to a paper titled Nicotine Dependence is Associated with Compulsive Alcohol Craving defines craving as “a psychological state characterized by obsessive thoughts and compulsive behavior” ( Hillemacher et al., 2006). The content of these thoughts is the urge to take the drug, and the compulsive behavior is addictive drug use. The source of these thoughts, according to most researchers interested in craving, is classical conditioning. For instance, conditioning creates an association between the pleasurable effects of using the drug and the stimuli that reliably predict access to the drug. When the addict re-encounters these stimuli, he or she is reminded of the pleasurable feelings, and this memory results in a powerful if not irresistible urge to take the drug. In support of this analysis, there is now a large experimental literature on the role of associative learning in craving and addiction ( Sayette et al., 2000 ; Tiffany and Carter, 1998). However, consider the possibility that craving also depends on its consequences. Assume that if craving is followed by access to the drug, then it is an instance of “savoring the drug,” which is pleasurable. Whereas, if craving is not followed by access to the drug then it generates feelings of disappointment and perhaps frustration and, as a result, decreases. These dynamics are not incompatible with the classical conditioning account of craving.
5.3. Evidence that smokers regulate their craving for cigarettes
Cigarette smoking offers an ideal preparation for studying the role of associative learning in craving. It is repetitive and often occurs in the same place. As predicted, smokers routinely report that craving is a key component of their addiction to cigarettes. Nevertheless, the following study suggests that craving is also maintained by its consequences.
Saul Shiffman and his colleagues at the University of Pittsburgh and Carnegie Mellon (1997) conducted an ambitious and highly informative account of the relationship between craving, quitting smoking, and relapse. The subjects were 240 smokers who wanted to quit and set a date for doing so. Several times a day, they recorded the strength of their desire to smoke in an electronic diary. On pre-quit days the average urge to smoke was relatively high. On the very first quit day, the average urge to smoke decreased, and it kept decreasing as days of abstinence increased. Surprisingly, there was little difference between the urge to smoke for those who resumed smoking (relapsed) and those who remained abstinent. (Most of the subjects resumed smoking.) However, as emphasized by Shiffman and his colleagues, on the morning that subjects relapsed, their urge to smoke was higher than on mornings of the previous days.
The results are consistent with the idea that the urge to smoke varied as a function of its consequences, which is to say, it was voluntary. Craving was highest in the pre-quit period when the participants could smoke at will, but then immediately decreased on the first quit day. As the decision to quit was voluntary, what seems to matter is the perceived availability of the drug. When the participants were most committed to not smoking, the urge to smoke significantly decreased. Why then did the urge to smoke increase somewhat on the day that the smokers resumed smoking? Perceived availability explains this if we assume that upon awakening the subjects had an inkling that they were going to resume smoking. According to this interpretation, craving accompanies drug use rather than precipitates drug use.
The Pittsburg study is valuable because of the relatively large number of subjects and that it was conducted outside of the lab. However, as a test of the capacity of addicts to regulate their cravings, it is limited. Cigarettes differ in many ways from other addictive drugs, and drug availability was under the control of the participants so that it was not a true independent variable. Although conducted some 16 years prior to the Pittsburg study, an experiment on the relationship between access to heroin and craving for heroin avoids these problems.
5.4. Evidence that heroin addicts regulate their drug cravings
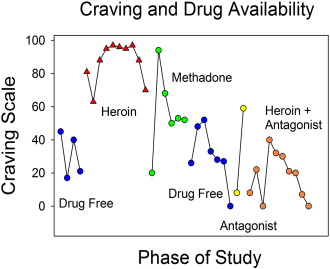
The study was conducted on a locked ward at McLean Hospital (Mirin, Meyer, McNamee, & McDougle, 1976). Five of the six subjects injected heroin daily prior to hospitalization. The researchers' goal was to evaluate the psychological effects of heroin as they occur, rather than depend on retrospective accounts. On specified days, the addicts could receive an injection of heroin at a dose of their choosing, provided that at least 2 h had passed since the previous dose. On other days, there were either no injections or heroin was combined with a drug that blocked its effects. Thus, access to heroin was under strict control. Fig. 3 shows the relationship between craving and type of day (access).
|
|
|
Fig. 3. Craving for heroin as a function of the availability of heroin. The subjects were six heroin addicts who resided on a locked ward at McLean Hospital. On the x-axis is the availability of heroin. On the y-axis is the craving score. The graph is based on the report by Mirin et al. (1976). |
Craving was highest on days that the subjects knew they could get heroin. Craving was lowest on days that no drug was available (“drug free”). On days that heroin was combined with a competitive agonist (methadone) or antagonist (naltrexone), craving levels were intermediate. This is precisely the pattern predicted by the idea that craving has hedonic consequences that, in turn, affect the likelihood of craving. Put in the language of reward and functional relations, the subjects learned to adjust their cravings in ways that made their stay on the ward more enjoyable and/or less aversive. In the language of free will, heroin addicts managed to adjust their cravings in order to crave heroin when it was available, but not crave heroin when it was pointless to do so. Notice, though, that this account is not as complete as it could be. Although heroin addicts regulated their cravings, it is not clear that they also had in mind the sort of desires that they wanted or did not want to have. That is, we do not know if they had “second-order” desires. Rather, the study shows that heroin addicts regulated their cravings for heroin and, thus, if called upon, could demonstrate Frankfurt’s version of free will.
We explored two empirical versions of free will in addicts: the ability to quit drugs, and the ability to adjust desires so that they coincide with the sort of desires that one wants to have. In both cases addicts met the test. This would seem to be the sort of “free will” worth having. Addicts can quit drugs; they can regulate their cravings; and they can adjust their desires to those that they want (should they have second-order desires).
6. Why is it so hard for addicts to quit drugs?
If addicts can regulate their cravings and quit taking drugs, why don't they just quit as soon as it becomes apparent that continuing to use drugs is a losing proposition? Or, as is sometimes said, “If it is just a choice then why not just quit.” One problem with this observation is that the phrase “just a choice” fails to reflect how difficult it is to do what is best. We have multiple allegiances, and they often dictate opposing choices. When the choice is to consume or not consume a drug, there are good reasons to do both, as described next.
6.1. Ambivalence
Drugs provide reliable, immediate and highly pleasurable changes in consciousness. To paraphrase one heroin user (Rettig, Torres, & Garrett, 1977), “On heroin you become your best you, its like Times Square and all the lights are flashing ‘yes’; kiss your worries goodbye; just an indescribable calm, nothing can hurt you.” For this young man nothing produced as much pleasure and as great a sense of well-being as getting high. To be sure, tolerance sets in and many drug users vainly chase the memory of their first high. But, intoxication need do no more than blunt some of the pain of everyday life to be preferred over sobriety. Putting these observations in economic terms may help the reader appreciate the allure of getting high.
From time to time, prices for medical care skyrocket, and there is the general impression that health care costs are too high. In contrast, prices for most staples are relatively stable, and there is the general impression that core staples are more likely to be fairly priced than is health care. According to economists these differences reflect, in part, the degree to which a good is essential and has substitutes. For instance, for most people there is no substitute for conventional medical care so that when ill, the alternatives are to pay the price the medical system sets or suffer. In an analogous fashion, intoxication is a unique psychological state that for many has few, if any, substitutes. This means that if intoxication remains the most desirable goal, drug use is the top choice, despite the mounting costs. Drugs corner the market on getting high, just as hospitals have cornered the market on medical cures.
But addictive drugs also have well-known, serious—sometimes fatal—liabilities. These include direct costs, such as overdose and withdrawal, and indirect socially mediated costs, such as legal problems, the disapproval of loved ones, health problems, and difficulties at work. Although on balance the costs exceed the benefits, the costs are uncertain and delayed. Most users never experience an overdose or contract lung cancer, and when negative effects do occur, they usually take years to emerge. Thus, addicts face a dilemma: immediately available, visceral positive experiences versus penalties that may never occur and are difficult to imagine. There are, of course, costs and benefits to most of what we do, but drugs create unusually difficult tradeoffs. For many addicts, the experienced benefits of quitting may not obviously outweigh the experienced benefits of continuing drug use. This makes it hard to quit.
6.2. Ambivalence as conflicting frames of reference
For some commodities, preference varies as a function of the frame of reference. For instance, imagine a regular smoker who has not had a cigarette for an hour or so. Putting all else aside, the next five minutes with a cigarette would be more enjoyable than the next five minutes without a cigarette. On the other hand, the same smoker is likely to prefer a longer rather than a shorter life and from this perspective she prefers not to smoke. There are two ways out of this dilemma. The smoker can reduce the immediate value of the cigarette (e.g., put on a nicotine patch), or she can reframe the next five minutes globally, as, for example, the first step toward better overall health. Both approaches must be relatively common given that most addicts eventually quit using drugs. Also notice that the local/global frame of reference dilemma is particularly acute for drugs. For instance, many enjoyable conventional activities—such as playing a musical instrument, reading a great book, skiing—provide both short-term and long-term benefits and as a result are less problematic.
7. Voluntary drug use does not imply that punishment is the appropriate “cure”
Although addicts are voluntary drug users, the claim that they should, therefore, be punished does not necessarily follow. Rather, the nature of voluntary behavior establishes a rationale for interventions that improve the welfare of addicts. This argument has not, to my knowledge, been made explicitly. Indeed, the opposite argument is the standard fare. An important debating point for the disease interpretation of addiction is that if addicts have a disease, we should search for a cure, but if they are voluntary users they should be punished. Of course it seems more enlightened and humane to search for a cure. First, I will point out helpful programs that involve neither pills nor pain and then provide a rationale for a non-punitive response to voluntary destructive behavior.
Contingency management programs and Alcoholics Anonymous employ neither penalties nor vaccines, yet both have proved effective as measured by reliable decreases in the symptoms of dependence (e.g., Davis et al., 2016 ; Vaillant, 2005). Although philosophically quite different, what the two approaches share are procedures that increase the value of nondrug activities and emphasis on the capacity of the addict to change. Ex-addict autobiographies make the same points. What is needed then are interventions that strengthen the addict’s capacity for voluntary positive action and access to viable nondrug alternatives.
7.1. A rationale for positive interventions for voluntary destructive behavior
Voluntary behavior depends on factors that are beyond individual control. Examples related to drug use include genetic based differences in drug metabolism (e.g., Luczak, Wall, Shea, Byun, & Carr, 2001), genetic based differences in impulsivity (Anokhin, Grant, Mulligan, & Heath, 2015), and genetic based differences in success in school (Belsky et al., 2016). Analogously, the local environment, as indexed by zip code, affects exposure to drugs during pregnancy (e.g., Brownsberger, 1997) and the opportunity to pursue economic and academic alternatives to drug use (e.g., Chetty et al., 2014 ; Warner et al., 1995). From the perspective that everyone deserves an equal chance for a good life, genetic and neighborhood based differences that abet destructive drug use are unfair. One solution is to introduce interventions that compensate for the disadvantages that so often accompany addiction. So even though addicts remain voluntary drug users, there are good reasons for affirmative interventions that do not necessarily involve punishment.
7.2. How to frame interventions: Attitude
Pickard (2011) provides a helpful example of a positive, non-pharmacological, non-punitive approach to addicts in a clinical setting. Her target audience is clinicians who work with personality disorder (PD) patients and addiction. The clinic “service users” are blameworthy. They routinely put their interests first in ways that harm others, they are duplicitous, and, in general, engender enmity and distrust from others. Yet, blame, says Pickard, is not clinically useful; what is needed are compassion and empathy. Thus, the clinician faces a dilemma: how to feel compassion for someone who deserves blame. Pickard suggests that the clinician take into account the addicts history:
One central way that clinicians can achieve compassion and empathy toward service users is simple: proper attention to service users' past history. As is well known, PD is associated with dysfunctional families… traumatic childhood experiences… PD service users often come from harrowing backgrounds, impoverished of all goods, to an extent that can be unimaginable to people who have not experienced these kinds of conditions.
Implicit in Pickards analysis is that (1) “PD service users” (and addicts) are not responsible for their traumatic childhood, (2) their current dysfunction reflects this past, and (3) thus they deserve empathy. This is precisely the point introduced in the just previous section: voluntary behavior depends on experiential and biological factors that are beyond individual control so that when these factors put someone at a disadvantage, the belief in equity motivates positive compensatory interventions.
7.3. How to frame interventions: Methods
The idea that drug use in addicts is voluntary has served as the basis for a number of treatment interventions. In the clinic, vouchers for abstinence improve outcomes for addicts seeking help to quit cocaine (Davis et al., 2016). In the workplace, drug testing programs that carry the threat of job loss yield an 80% to 100% decrease in drug use (e.g., Coombs, 1997 ; Heyman, 2009). In the justice system, the Project HOPE contingency program reduced drug use in criminal offenders who were on parole by 72% (Hawken & Kleiman, 2009).
8. Conclusion
I evaluated two empirical interpretations of free will: Can addicts stop being addicts and can addicts regulate their desire to take drugs so that it coincides with their second-order desire to be someone who does not desire drugs? Fig. 1 ; Fig. 2 showed that addiction to illicit drugs typically ended within a few years, and memoirs, field research, and the historical record agree that these changes occurred voluntarily, usually without the assistance of treatment programs. For alcoholics and smokers, addiction lasted considerably longer, but as with illicit drugs, most legal drug users are on record as no longer dependent, and the estimated asymptotic recovery levels were above 90%. Analogously, research reveals that addicts can regulate their cravings. This helps establish the necessary conditions for an addict who wants to be someone who doesn’t crave drugs. On the basis of the criteria used in this report, addicts have free will.
It is time to change how we talk about addiction. The results displayed in Fig. 1, Fig. 2 ; Fig. 3 and similar findings deserve more attention. The success and implications of contingency management interventions deserve more attention (Davis et al., 2016). There are many reasons why people use drugs in harmful ways, but compulsivity is not one of them. What the research shows is that addicts retain the capacity to say “no” to drugs and most do so.
Acknowledgements
I thank Gerald Zuriff and Hanna Pickard for their helpful comments and Verna Mims for her helpful comments and expert assistance in preparing this manuscript.
References
- Ainslie, 2013 G. Ainslie; Intertemporal bargaining in addiction; Frontiers in Psychiatry, 4 (2013) https://doi.org/10.3389/fpsyt.2013.00063
- American Psychiatric Association, 1994 American Psychiatric Association; Diagnostic and statistical manual of mental disorders: DSM-IV; (4th ed.)Author, Washington, D.C. (1994)
- Anokhin et al., 2015 A.P. Anokhin, J.D. Grant, R.C. Mulligan, A.C. Heath; The genetics of impulsivity: Evidence for the heritability of delay discounting; Biological Psychiatry, 77 (2015), pp. 887–894
- Anthony and Helzer, 1991 J.C. Anthony, J.E. Helzer; Syndromes of drug abuse and dependence; L.N. Robins, D.A. Regier (Eds.), Psychiatric disorders in America: The epidemiologic catchment area study, Free Press, New York (1991), pp. 116–154
- Belsky et al., 2016 D.W. Belsky, T.E. Moffitt, D.L. Corcoran, B. Domingue, H. Harrington, S. Hogan, ... A. Caspi; The genetics of success: How single-nucleotide polymorphisms associated with educational attainment relate to life-course development; Psychological Science, 27 (2016), pp. 957–972
- Biernacki, 1986 P. Biernacki; Pathways from heroin addiction: Recovery without treatment; Temple University Press, Philadelphia (1986)
- Brownsberger, 1997 W.N. Brownsberger; Prevalence of frequent cocaine use in urban poverty areas; Contemporary Drug Problems, 24 (1997), pp. 349–371
- Chetty et al., 2014 R. Chetty, N. Hendren, P. Kline, E. Saez, N. Turner; Is the United States still a land of opportunity? Recent trends in intergenerational mobility; The American Economic Review, 104 (2014), pp. 141–147
- Chiten et al., 1994 L. Chiten, P. Medley, B. Russel; Twitch and shout: A documentary about Tourette syndrome; S.l, Twitch and Shout Productions (1994)
- Colón et al., 2002 H.M. Colón, R.R. Robles, H. Sahai; The validity of drug use self-reports among hard core drug users in a household survey in Puerto Rico: Comparison of survey responses of cocaine and heroin use with hair tests; Drug and Alcohol Dependence, 67 (2002), pp. 269–279
- Conway et al., 2006 K.P. Conway, W. Compton, F.S. Stinson, B.F. Grant; Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: Results from the National Epidemiologic Survey on alcohol and related conditions; Journal of Clinical Psychiatry, 67 (2006), pp. 247–257
- Coombs, 1997 R.H. Coombs; Drug-impaired professionals; Harvard University Press, Cambridge, MA (1997)
- Courtwright, 1982 D.T. Courtwright; Dark paradise: Opiate addiction in America before 1940; Harvard University Press, Cambridge, MA (1982)
- Davis et al., 2016 D.R. Davis, A.N. Kurti, J.M. Skelly, R. Redner, T.J. White, S.T. Higgins; A review of the literature on contingency management in the treatment of substance use disorders, 2009–2014; Preventive Medicine, An International Journal Devoted To Practice And Theory (2016), pp. 9236–9246 https://doi.org/10.1016/j.ypmed.2016.08.008
- Darke, 1998 S. Darke; Self-report among injecting drug users: A review; Drug and Alcohol Dependence, 51 (1998), pp. 253–263
- Frankfurt, 1971 H.G. Frankfurt; Freedom of the will and the concept of a person; Journal of Philosophy, 68 (1971), pp. 5–20
- Gossop et al., 2003 M. Gossop, J. Marsden, D. Stewart, T. Kidd; The National Treatment Outcome Research Study (NTORS): 4–5 year follow-up results; Addiction, 98 (2003), pp. 291–303
- Hailman, 1969 J.P. Hailman; How an instinct is learned; Scientific American, 221 (1969), pp. 98–106
- Hart, 2013 C. Hart; High price: A neuroscientists journey of self-discovery that challenges everything you know about drugs and society; Hearper Collins (2013)
- Hawken and Kleiman, 2009 A. Hawken, M. Kleiman; Managing drug involved probationers with swift and certain sanctions: Evaluating Hawaiis HOPE: Executive summary; (2009) Report submitted to the National Institute of Justice. http://www.ncjrs.gov/pdffiles1/nij/grants/229023.pdf
- Heather and Segal, 2016 N. Heather, G. Segal (Eds.), Addiction and choice: Rethinking the relationship, Oxford University Press (2016)
- Heyman, 2009 G.M. Heyman; Addiction: A disorder of choice; Harvard University Press, Cambridge (2009)
- Heyman, 2013 G.M. Heyman; Quitting drugs: Quantitative and qualitative features; Annual Review of Clinical Psychology, 9 (2013), pp. 29–59
- Heyman and Mims, 2016 G.M. Heyman, V. Mims; What addicts can teach us about addiction: A natural history approach; N. Heather, G. Segal (Eds.), Addiction and choice: Rethinking the relationship, Oxford University Press, Oxford (2016)
- Higgins et al., 2000 S.T. Higgins, C.J. Wong, G.J. Badger, D.E. Ogden, R.L. Dantona; Contingent reinforcement increases cocaine abstinence during outpatient treatment and 1 year of follow-up; Journal of Consulting and Clinical Psychology, 68 (2000), pp. 64–72
- Hillemacher et al., 2006 T. Hillemacher, K. Bayerlein, J. Wilhelm, H. Frieling, N. Thürauf, M. Ziegenbein, ... S. Bleich; Nicotine dependence is associated with compulsive alcohol craving; Addiction, 101 (2006), pp. 892–897
- James, 2013 W. James; The principles of psychology; Read Books Ltd. (2013/1890)
- Kessler et al., 2005 R.C. Kessler, W.T. Chiu, O. Demler, K.R. Merikangas, E.E. Walters; Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication; Archives of General Psychiatry, 62 (2005), pp. 617–627
- Kolb and DuMez, 1981 L. Kolb, A.G. DuMez; Prevalence and trends of drug addiction in the United States and factors influencing it (public health reports, v. 39, no. 21); G.N. Grob (Ed.), Public policy and the problem of addiction: Four studies, 1914–1924, Arno Press, New York (1981/1924)
- Ledgerwood et al., 2008 D.M. Ledgerwood, B.A. Goldberger, N.K. Risk, C.E. Lewis, R. Kato Price; Comparison between self-report and hair analysis of illicit drug use in a community sample of middle-aged men; Addictive Behaviors, 33 (2008), pp. 1131–1139
- Leshner, 1997 A.I. Leshner; Addiction is a brain disease, and it matters; Science, 278 (1997), p. 45
- Lewis, 2015 M. Lewis; The biology of desire: Why addiction is not a disease; PublicAffairs (2015)
- Lopez-Quintero et al., 2011 C. Lopez-Quintero, D.S. Hasin, J.P. de Los Cobos, A. Pines, S. Wang, B.F. Grant, C. Blanco; Probability and predictors of remission from life-time nicotine, alcohol, cannabis or cocaine dependence: Results from the National Epidemiologic Survey on Alcohol and Related Conditions; Addiction, 106 (2011), pp. 657–669
- Luczak et al., 2001 S.E. Luczak, T.L. Wall, S.H. Shea, S.M. Byun, L.G. Carr; Binge drinking in Chinese, Korean, and White college students: Genetic and ethnic group differences; Psychology of Addictive Behaviors, 15 (2001), pp. 306–309
- McLellan et al., 2000 A.T. McLellan, D.C. Lewis, C.P. O'Brien, H.D. Kleber; Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation; JAMA: The Journal of the American Medical Association, 284 (2000), pp. 1689–1695
- Mirin et al., 1976 S.M. Mirin, R.E. Meyer, H.B. McNamee, M. McDougle; Psychopathology, craving, and mood during heroin acquisition: An experimental study; International Journal of the Addictions, 11 (1976), pp. 525–544
- Miron and Zwiebel, 1991 J.A. Miron, J. Zwiebel; Alcohol consumption during prohibition; American Economic Review, 81 (1991), pp. 242–247
- O'Brien and McLellan, 1996 C.P. O'Brien, A.T. McLellan; Myths about the treatment of addiction; Lancet, 347 (1996), pp. 237–240
- Palmer et al., 2015 R.C. Palmer, L. Brick, N.R. Nugent, L.C. Bidwell, J.E. McGeary, V.S. Knopik, M.C. Keller; Examining the role of common genetic variants on alcohol, tobacco, cannabis and illicit drug dependence: Genetics of vulnerability to drug dependence; Addiction, 110 (2015), pp. 530–537
- Perry et al., 2013 C.J. Perry, A.B. Barron, K. Cheng; Invertebrate learning and cognition: Relating phenomena to neural substrate; WIREs Cognitive Science, 4 (5) (2013), pp. 561–582 https://doi.org/10.1002/wcs.1248
- Pickard, 2011 H. Pickard; Responsibility without blame: Empathy and the effective treatment of personality disorder; Philosophy, Psychiatry, & Psychology: PPP, 18 (2011), p. 209
- Pickard, 2017 H. Pickard; Addiction; K. Timpe, M. Griffith, N. Levy (Eds.), The Routledge Companion to Free Will, Routledge, New York (2017)
- Regier et al., 1990 D.A. Regier, M.E. Farmer, D.S. Rae, B.Z. Locke, S.J. Keith, L.L. Judd, F.K. Goodwin; Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) study; JAMA: The Journal of the American Medical Association, 264 (1990), pp. 2511–2518
- Rettig et al., 1977 R.P. Rettig, M.J. Torres, G.R. Garrett; Manny: A criminal-addicts story; University of California, Houghton Mifflin (1977)
- Robins, 1993 L.N. Robins; Vietnam veterans' rapid recovery from heroin addiction: A fluke or normal expectation?; Addiction, 88 (1993), pp. 1041–1054
- Robins and Murphy, 1967 L.N. Robins, G.E. Murphy; Drug use in a normal population of young negro men; American Journal of Public Health and the Nations Health, 57 (1967), pp. 1580–1596
- Robinson et al., 2001 T.E. Robinson, G. Gorny, E. Mitton, B. Kolb; Cocaine self-administration alters the morphology of dendrites and dendritic spines in the nucleus accumbens and neocortex; Synapse, 39 (2001), pp. 257–266
- Rounsaville et al., 1991 B.J. Rounsaville, S.F. Anton, K. Carroll; Psychiatric diagnoses of treatment-seeking cocaine abusers; Archives of General Psychiatry, 48 (1991), pp. 43–51
- Sayette et al., 2000 M.A. Sayette, S. Shiffman, S.T. Tiffany, R.S. Niaura, C.S. Martin, W.G. Shadel; The measurement of drug craving; Addiction, 95 (Suppl. 2) (2000), pp. S189–S210
- Seeley, 1960 J.R. Seeley; Death by liver cirrhosis and the price of beverage alcohol; Canadian Medical Association Journal, 83 (1960), pp. 1361–1366
- Shiffman et al., 1997 S. Shiffman, J.B. Engberg, J.A. Paty, W.G. Perz, M. Gnys, J.D. Kassell, M. Hickcox; A day at a time: Predicting smoking lapse from daily urge; Journal of Abnormal Psychology, 106 (1997), pp. 104–116
- Sinnott-Armstrong and Pickard, 2013 W. Sinnott-Armstrong, H. Pickard; What is addiction; Oxford Handbook of Philosophy of Psychiatry (2013), pp. 851–864
- Stinson et al., 2005 F.S. Stinson, B.F. Grant, D. Dawson, W.J. Ruan, B. Huang, T. Saha; Comorbidity between DSM-IV alcohol and specific drug use disorders in the United States: Results from the National Epidemiological Survey on alcohol and related conditions; Drug and Alcohol Dependence, 80 (2005), pp. 105–116
- Tiffany and Carter, 1998 S.T. Tiffany, B.L. Carter; Is craving the source of compulsive drug use?; Journal of Psychopharmacology, 12 (1998), pp. 23–30
- Toneatto et al., 1999 T. Toneatto, L.C. Sobell, M.B. Sobell, E. Rubel; Natural recovery from cocaine dependence; Psychology of Addictive Behaviors, 13 (1999), pp. 259–268
- U.S. Department of Health and Human Services, 1994 U.S. Department of Health & Human Services; Cigarette smoking among adults in the US, 1993; Morbidity and Mortality Weekly Review43 (1994), pp. 925–930
- U.S. Department of Health and Human Services, 1990 U.S. Department of Health & Human Services; The health benefits of smoking cessation, a report of the surgeon general; U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office of Smoking and Health (1990) (DHHS Publication No. (CDC) 90-8416)
- Vaillant, 2005 G.E. Vaillant; Alcoholics anonymous: Cult or cure?; Australian and New Zealand Journal of Psychiatry, 39 (2005), pp. 431–436
- Volkow, 2015 N.D. Volkow; https://www.drugabuse.gov/about-nida/noras-blog/2015/06/addiction-disease-free-will (2015)
- Waldorf et al., 1991 D. Waldorf, C. Reinarman, S. Murphy; Cocaine changes: The experience of using and quitting; Temple University Press, Philadelphia (1991)
- Wang et al., 2016 L. Wang, F. Zou, T. Zhai, Y. Lei, S. Tan, X. Jin, ... Z. Yang; Abnormal gray matter volume and resting-state functional connectivity in former heroin-dependent individuals abstinent for multiple years; Addiction Biology, 21 (3) (2016), pp. 646–656 https://doi.org/10.1111/adb.12228
- Warner, 1994 J. Warner; ‘Resolv'd to drink no more’: Addiction as a preindustrial construct; Journal of Studies on Alcohol, 55 (1994), pp. 685–691
- Warner et al., 1995 L.A. Warner, R.C. Kessler, M. Hughes, J.C. Anthony, C.B. Nelson; Prevalence and correlates of drug use and dependence in the United States; Results from the National Comorbidity Survey 52, Archives of General Psychiatry (1995), pp. 219–229
- Wasserman et al., 1998 D.A. Wasserman, M.G. Weinstein, B.E. Havassy, S.M. Hall; Factors associated with lapses to heroin use during methadone maintenance; Drug and Alcohol Dependence, 52 (1998), pp. 183–192
- Weatherby et al., 1994 N.L. Weatherby, R. Needle, H. Cesari, R. Booth, C.B. McCoy, J.K. Watters, ... D.D. Chitwood; Validity of self-reported drug use among injection drug users and crack cocaine users recruited through street outreach; Evaluation and Program Planning, 17 (1994), pp. 347–355
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?