Abstract
Vascular injuries associated with the tibial nailing have been reported in few case reports. We here report a unique case of anterior tibial artery (ATA) pseudoaneurysm caused by the second proximal coronal interlocking bolt. We found that the position of interlocking bolts on the nail brings them very close to the anatomical positions of arteries in leg. The reports of ATA injury by interlocking bolts highlight the need for reconsidering the nail design and screw hole positions.
Keywords
Interlocking screw ; Tibia nailing ; Pseudoaneurysm ; Anterior tibial artery ; Vascular injury ; Trauma
Introduction
Several modalities have been used in the treatment of tibial diaphyseal fractures. However the most commonly used modality nowadays is intra-medullary nailing. There has been reports of vascular injury with the use of intra-medullary nail.1 ; 2 ; 3 ; 4 ; 5 ; 6 ; 7 We here report a case of a 60- year-old male with a closed tibia fracture treated with an intra-medullary tibial nail which developed an anterior tibial artery pseudoaneurysm 6 months after the surgery. This is only the second case in English literature of anterior tibial artery pseudoaneurysm due to the coronal proximal locking screws of tibial intramedullary nail, the first one reported by Inamdar et al.4
Case details
A 60 year male was referred to our institute with swelling and pain in the right calf since last one month. Patient gave history of road traffic accident 6 month back during which he sustained injury to his right leg. He was diagnosed with fracture tibia then at a peripheral hospital, where Intra-medullary nailing (closed) was done. The patient was started with passive and active assisted range of motion exercises for knee and partial weight bearing after two days with help of crutches. He was then transferred to full weight bearing walking after 4 weeks with stick. Patient had been walking normally without support for the past 3 months.
1 month back patient started developing swelling in the proximal third of leg on the lateral aspect. The swelling kept on gradually progressing in size, along with increasing pain and tenderness. Thinking it might be due to pus formation and infection, an attempt was made to drain it at a peripheral hospital. The futile attempt however yielded only blood and clots. The swelling kept on increasing in size causing the incision to dehisce and gape later on (Fig. 1 ).
|
|
|
Fig. 1. Clinical photo showing the gaping wound at the time of presentation to our institute. |
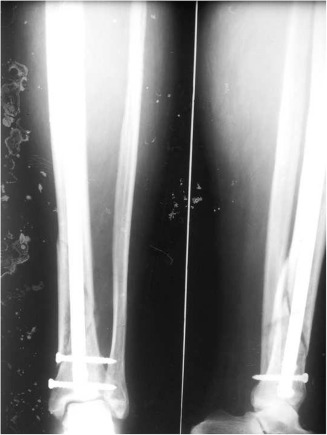
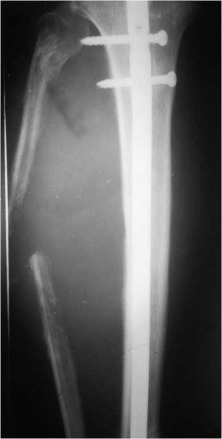
On the first presentation to our institute, physical examination revealed tender swelling with a gaping wound in the proximal half of the leg along with common peroneal nerve palsy. Dorsalis pedis pulse, although palpable, was feeble and reduced in volume as compared to the opposite side; posterior tibial pulses were normal though. Sequential roentograms which the patient had got done before coming to us, showed fracture tibia with intramedullary nail along with rarefaction and dissolution of fibula. A soft tissue swelling expanding laterally and pushing the fibula outwards and dissolving it in the process could be seen (Fig. 2 , Fig. 3 ; Fig. 4 ).
|
|
|
Fig. 2. Radiograph done 2 weeks after the primary surgery (nailing). Slight haziness and whiteness of soft tissues is seen in proximal part. |
|
|
|
Fig. 3. Radiograph done 4 weeks after primary surgery (nailing). Lateral expansion of the fibula erosion of the cortex seen on both tibia and fibula. |
|
|
|
Fig. 4. Radiograph at the time of case presentation to our hospital. The erosion and expansion have progressed with thinning of fibula. |
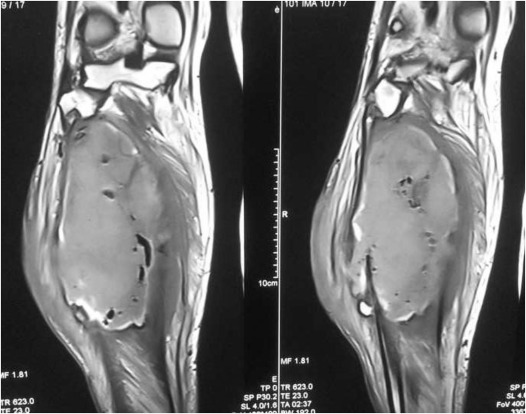
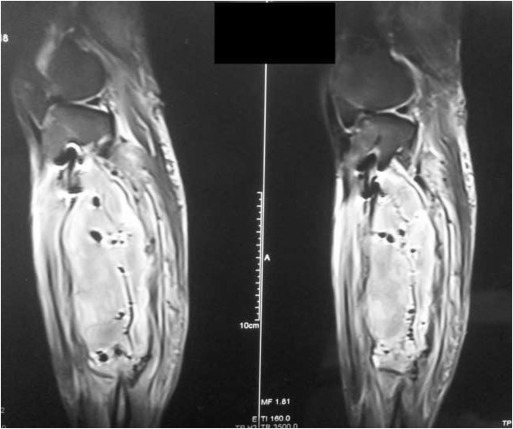
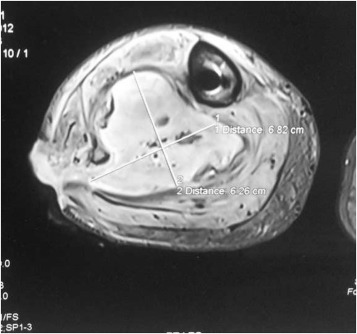
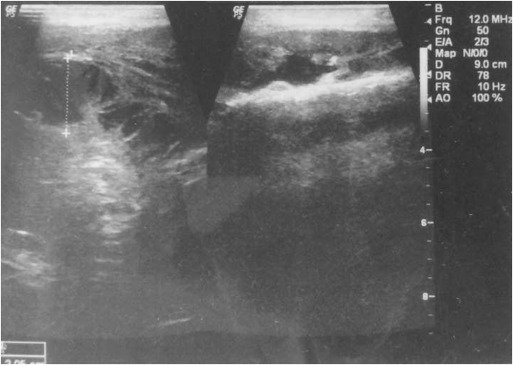
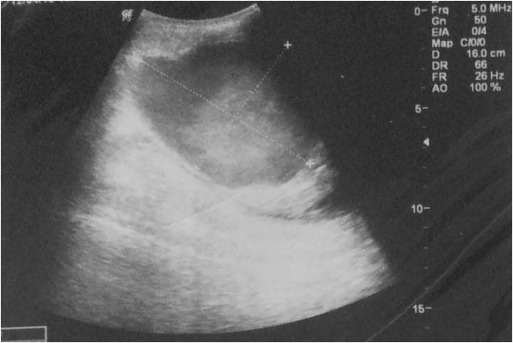
The patient was evaluated by both vascular surgery and orthopaedic teams. MRI revealed a soft tissue swelling due to hematoma in the posterolateral aspect of calf. Size of the hematoma was around about 16 cm vertically, 7 cm mediolaterally and 6.2 cm antero-posteriorly at the maximum width (Fig. 5 , Fig. 6 ; Fig. 7 ). Doppler Ultrasound also showed hematoma with feeding artery in the wall of cavity (Fig. 8 ; Fig. 9 ). Decision was taken to explore the wound inside operation theatre for any active bleed. Around 500 ml of clot was found in calf region within a well-defined cavity which was evacuated. We did not find any active bleeder in the cavity although anterior tibial was palpable in the wall of cavity. To prevent any future bleeds, anterior tibial artery embolization by coils was done by digital subtraction angiography (DSA), post-embolisation angiogram showed no extravasation. Post-operatively the limb was warm and viable. We performed the CT angiography and the embolisation of artery in the same sitting.
|
|
|
Fig. 5. MRI T1 image, coronal section, showing the soft tissue mass in the posterior compartment of leg. |
|
|
|
Fig. 6. MRI T2 image, sagittal section, showing the hyper-echoic mass and the close proximity of proximal locking bolts. The hematoma is seen to extend well to the middle of leg. |
|
|
|
Fig. 7. MRI T2 image, axial section, at the level of maximum thickness of the mass to measure the dimensions. |
|
|
|
Fig. 8. Ultrasound images to see the relation of hematoma to the surrounding structures and evaluate the origin. |
|
|
|
Fig. 9. Ultrasound images to see the relation of hematoma to the surrounding structures and evaluate the origin. |
Patient was followed up for any swelling or pain at 12 months and 18 months, none was present and the patient was walking without aid. Radiographs show gradual healing response of fibula (Fig. 11 ; Fig. 12 ) and the wound healed uneventfully (Fig. 10 ). The peroneal nerve had recovered fully at the last visit with active dorsiflexion present.
|
|
|
Fig. 10. Follow up 12 months clinical picture showing complete healing with subsidence of swelling. |
|
|
|
Fig. 11. 12 months follow-up radiograph showing calcification of fibula. The intravascular coil can be seen near the fibular neck. |
|
|
|
Fig. 12. 18 months follow-up radiograph showing near complete normalization of fibula. |
Discussion
Pseudoaneurysms are false aneurysms which have a wall of fibrous tissue, instead of the normal arterial wall characteristic of the true aneurysms. They are formed when a rent is produced in the arterial wall which bleeds out slowly in the surrounding tissues. This creates an enlarging hematoma. Most of the time, the blood flow is maintained through the parent artery, hence patent pulses are found on physical examination.8 Symptoms produced by a traumatic aneurysm are mostly due pressure on the surrounding structures causing pain, numbness or muscle weakness distal to the lesion due to pressure on the nerves.
Pseudoaneurysms of anterior tibial artery have been reported previously to occur secondary to trauma in leg, tibial fracture, ankle arthroscopy, ankle sprain and after placement of illizarov fixator.9 ; 10 ; 11 ; 12 ; 13 Vascular injury due to interlocking bolts in cases where tibial nailing was done have been reported in few case reports (Table 1 ). We found only one case report of anterior tibial artery pseudoaneurysm due to proximal medio-lateral interlocking screw (coronal plane) of tibial intramedullary nail.4 Inamdar et al4 have reported a 30 year old male patient who sustained a closed tibia fracture which was fixed by closed intramedullary nailing (Grosse and Kempf nail). Their patient complained of enlarging swelling on lateral aspect of upper third of same leg at the end of one year after surgery. It was diagnosed as pseudoaneurysm arising from the anterior tibial artery after investigating with Doppler ultrasound and angiogram. The authors have reported an audible bruit and pulsation in the swelling, which was not present in our case. The nail was removed and the anterior tibial artery was ligated in the wall of the cavity. The authors also removed the fibular head along with 8 cm of proximal fibula.4
| Author | Patients | Site of arterial injury | Locking bolt involved with injury | Management | |
|---|---|---|---|---|---|
| 1 | Williamson and Kershaw19 1989 | 1 | Popliteal artery laceration | Proximal sagittal bolt | Arterial repair with vein autograft |
| 2 | Urban and Tornetta7 1995 | 1 | Distal ATA impingement | Distal medial to lateral bolt | Screw backed out a bit and later removed |
| 3 | Mehta et al5 2003 | 1 | Distal ATA impingement | Distal medial to lateral bolt | Screw exchange and reinsertion of smaller screw |
| 4 | Kyeoung- jin hon et al2 2004 | 1 | Distal ATA pseudoaneurysm | Distal lateral to medial bolt | Excision of pseudoaneurysm, autograft repair of artery. Screw reinsertion from medial to lateral |
| 5 | Inamdar et al4 2005 | 1 | Proximal ATA pseudoaneurysm | Proximal lateral to medial bolt | Nail removal, excision of proximal fibula & pseudoaneurysm. Ligation of ATA. |
| 6 | Hussain et al3 2011 | 1 | Popliteal artery laceration | Proximal Medial to lateral oblique bolt | Primary arterial repair |
| 7 | Bono et al1 2013 | 16 legs (cadaveric study) | Distal AP bolts | Conclusion: Distal AP bolts are in close proximity to neurovascular bundle |
ATA: anterior tibial artery, AP: anteroposterior.
In our case, we performed the DSA coiling of anterior tibial artery to prevent any future bleeds, but only after confirming the patency of posterior tibial and peroneal arteries. We think the arterial injury might have been caused during the drilling of the screw by power drill causing a small longitudinal rent in arterial wall, which later caused the pseudoaneurysm. As the fracture level was also lower than the aneurysm site, we could not find any other reason for the expanding aneurysm in an otherwise asymptomatic patient.
The position of the distal screw out of the two proximal screws places it very near to the anterior tibial artery, making it a potential source of injury during drilling or due to long screws lengths. The anterior tibial artery is a branch of popliteal artery arising at the distal border of the popliteus muscle. It then enters the anterior compartment by hooking over the proximal border of the interosseous membrane, approximately at the level of the fibular head. This peculiar course makes the artery relatively fixed here, reducing mobility and hence making it prone to injury.14 A high origin ATA is diagnosed when the popliteal artery branches above the level of popliteus muscle and the ATA passes anterior to the popliteus muscle, in direct contact with the posterior tibial cortex. This peculiar course puts it at risk in procedures of proximal tibia like osteotomy or knee replacement surgeries, as pointed out by Tindall et al15 who studied the surgical significance of the high origin ATA. The authors used the Duplex ultrasound imaging for evaluating the arterial course as in addition to being a quick non-invasive modality to study vascular anatomy, it also shows the adjacent muscles and structures more clearly than the angiography.15 Day and Orme16 studied the normal anatomy of the popliteal artery and its branching patterns in 568 patients by angiography. They reported that 90.7% patients had the normal branching pattern of the popliteal artery i.e. anterior tibial artery arises first and then posterior tibial and peroneal arteries arise from the common tibial-peroneal trunk. 9.3% limbs showed anatomic variations in the branching pattern, of which the most common were a high arising ATA (4.5% limbs) or trifurcation of popliteal artery (3.2% limbs) with simultaneous origin of all three arteries.
Although we did not find any anatomic variation in ATA course in our study; we think that such a variation would not pose any problems during coronal locking bolts placement as their position is much inferior, but it might be important in nails with sagittal proximal screws. We measured the distance of the second hole on proximal part of tibial nail from the upper end of nail, it came at around 6 cm (Fig. 13 ). This places the second screw at the level of fibular neck, dangerously close to the anterior tibial artery (Fig. 2 ; Fig. 12 ). Suri et al17 have reported a pseudoaneurysm of anterior tibial artery due to a more posteriorly placed stienmann pin through proximal tibia for the purpose of skeletal traction. Their finding also supports our concern for the vulnerability of ATA in this area.
|
|
|
Fig. 13. Distance of screws from the upper nail-end. |
Several technical points are worth mentioning while putting the proximal medial to lateral locking bolts. Firstly, as the bone of proximal tibia more cancellous at the site of screw placement, the surgeon might not feel the typical change in pitch or sensation of far cortex breach, which is common in cortical bone drilling.1 So take use of intraoperative fluoroscopy to prevent overdrilling into the far soft tissues where the artery lies. Another thing which can be done is to use oscillating drill or put drill in reverse while drilling the far cortex.3 Although ideal would be to do preoperative Doppler ultrasound or angiography to make note of arterial course, but we agree that is not possible in every case due to the different hospital conditions and emergency situations. The screw length should not be more than required for good hold, just tip outside of bone with first few threads engaging the far cortex, intraoperative radiography should be used to check that. Although we could not find any specific visual marker to indirectly know the arterial position, but the various studies quote ATA to pass near the neck of fibula,15 ; 18 which is approximately the level of second proximal screw. Hence there is always a chance of damage to artery while drilling or measuring screw length or putting longer screw. In our case the screw is a bit longer, with 2/3 threads outside the far cortex. This might have led to the pseudoaneurysm formation in our case.
Taking into consideration the other case reports of vascular injury by proximal screws of tibia nail, we propose either a change in the level of the second screw by bringing it more proximal in the region of proximal tibial metaphysis above the arterial trifurcation. Since at that level popliteal artery is posterior to popliteus muscle in midline, we have a safer zone for screw placement. Also a coronal plane is safer option than sagittal plane for screw placement.
Conclusion
We think the position of the second proximal screw is very precarious and places it dangerously close to the anterior tibial artery hence increasing the chances of vascular injury. Care should be taken while drilling to prevent injury to artery. The screw hole on the nail can be moved proximally on the nail so that screw takes hold in the tibial metaphysis. Also coronal plane is a safer plane than the sagittal plane to prevent vascular injury.
References
- 1 C.M. Bono, M. Sirkin, C.T. Sabatino, M.C. Reilly, I. Tarkin, F.F. Behrens; Neurovascular and tendinous damage with placement of anteroposterior distal locking bolts in the tibia; J Orthop Trauma, 17 (10) (2003 Nov- Dec), pp. 677–682 PubMed PMID: 14600566
- 2 K.J. Han, Y.Y. Won, S.Y. Khang; Pseudoaneurysm after tibial nailing; Clin Orthop Relat Res, 418 (2004 Jan), pp. 209–212 PubMed PMID: 15043118
- 3 W. Hussain, T. Balach, J.M. Leland; Vascular injury involving proximal medial-to-lateral oblique locking screw insertion in tibial intramedullary nailing; Acta Orthop Belg, 77 (3) (2011 Jun), pp. 414–418 PubMed PMID: 21846016
- 4 D. Inamdar, M. Alagappan, L. Shyam, S. Devadoss, A. Devadoss; Pseudoaneurysm of anterior tibial artery following tibial nailing: a case report; J Orthop Surg (Hong Kong), 13 (2) (2005 Aug), pp. 186–189 PubMed PMID: 16131685
- 5 S. Mehta, C. Cumins, R. Milgram; Anterior tibial artery impingement by a distal interlocking screw: a case report; Univ Pa Orthop J, 16 (2003), pp. 35–37
- 6 A.A. Shetty, A.J. Tindall, F. Qureshi, M. Divekar, K.W. Fernando; The effect of knee flexion on the popliteal artery and its surgical significance; J Bone Jt Surg Br, 85 (2) (2003 Mar), pp. 218–222 PubMed PMID: 12678356
- 7 W.P. Urban Jr., P. Tornetta 3rd; Vascular compromise after intramedullary nailing of the tibia: a case report; J Trauma, 38 (5) (1995 May), pp. 804–807 PubMed PMID: 7760413
- 8 F.C. Spencer, A.M. Imparato; S.I. Schwartz, R.C. Lillehei, G.T. Shires, F.C. Spencer, E.H. Storer (Eds.), Peripheral Arterial Disease (2nd ed.), McGraw Hill, New York (1969)
- 9 G.M. Vincent, W.D. Stanish; False aneurysm after arthroscopic meniscectomy. A report of two cases; J Bone Jt Surg Am, 72 (5) (1990 Jun), pp. 770–772 PubMed PMID: 2355041
- 10 R. Biermann, M. Novak; False aneurysm of the anterior tibial artery as a sequela of complicated foreleg fracture; Rozhl Chir, 69 (6) (1990 Jun), pp. 396–400 PubMed PMID: 2237656. Anaeurysma spurium arteria tibialis anterior ako nasledok komplikovanej zlomeniny kosti predkolenia
- 11 W. Braito, C. Montanari, F. Caracciolo, G. Paroni, G. Domenella; False aneurysm of the anterior tibial artery in lower leg fractures treated with the Ilizarov external fixator. Case report; Ital J Orthop Traumatol, 18 (1) (1992), pp. 135–139 PubMed PMID: 1399529
- 12 R.Q. Crellin, M.J. Tsapogas; Traumatic aneurysm of the anterior tibial artery. Report of a case; J Bone Jt Surg Br, 45-B (1963 Feb), pp. 142–144 PubMed PMID: 14041406
- 13 C.J. Salgado, D. Mukherjee, M.A. Quist, S. Cero; Anterior tibial artery pseudoaneurysm after ankle arthroscopy; Cardiovasc Surg, 6 (6) (1998 Dec), pp. 604–606 PubMed PMID: 10395264
- 14 S. Starling, H. Ellis; Gray’s Anatomy. The Anatomical Basis of Clinical Practice; Churchill Livingstone, Edinburgh (2005)
- 15 A.J. Tindall, A.A. Shetty, K.D. James, A. Middleton, K.W. Fernando; Prevalence and surgical significance of a high-origin anterior tibial artery; J Orthop Surg (Hong Kong), 14 (1) (2006 Apr), pp. 13–16 PubMed PMID: 16598080
- 16 C.P. Day, R. Orme; Popliteal artery branching patterns – an angiographic study; Clin Radiol, 61 (8) (2006 Aug), pp. 696–699 PubMed PMID: 16843754
- 17 T. Suri, V. Dabas, S. Sural, A. Dhal; Pseudoaneurysm of the anterior tibial artery: a rare complication of proximal tibial steinman pin insertion; Indian J Orthop, 45 (2) (2011 Mar), pp. 178–180 PubMed PMID: 21430875. Pubmed Central PMCID: 3051127
- 18 S. Yildiz, F. Yazar, H. Ozan; A high-origin anterior tibial artery and its current clinical importance; Int J Anat Var, 3 (2010), pp. 180–182
- 19 D.M. Williamson, C.J. Kershaw; Serious vascular complication of locked tibial nailing; Injury, 20 (5) (1989 Sep), pp. 310–312 PubMed PMID: 2613323
Document information
Published on 31/03/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?