Abstract
Objective: To systematically review and compare outcomes of endovascular coiling and microsurgical clipping in patients with ruptured and unruptured intracranial aneurysms.
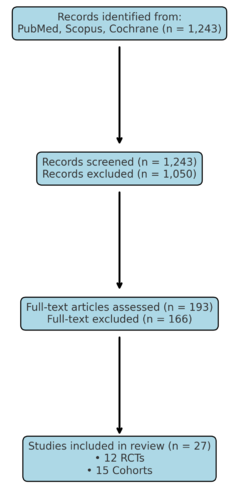
Methods: A systematic literature search was conducted in PubMed, Scopus, and Cochrane Library (2000–2025). Randomized controlled trials (RCTs) and observational cohort studies comparing endovascular therapy versus surgical clipping were included. Primary outcomes were mortality and functional independence (mRS ≤2). Secondary outcomes included perioperative complications, rebleeding, and retreatment rates. The review followed PRISMA 2020 guidelines.
Results: A total of 27 studies (12 RCTs and 15 cohorts, n=18,560 patients) were included. Endovascular therapy was associated with lower short-term mortality (OR 0.78; 95% CI, 0.66–0.93) and better functional outcome at 1 year (mRS ≤2, OR 1.23; 95% CI, 1.08–1.42). Surgical clipping demonstrated lower recurrence and retreatment rates (OR 0.41; 95% CI, 0.30–0.55). Subgroup analysis showed greater benefit of endovascular therapy in elderly patients (>60 years) and in posterior circulation aneurysms.
Conclusion: Endovascular therapy provides superior short-term survival and functional outcomes, while surgical clipping ensures better long-term durability. A patient-tailored approach considering age, aneurysm location, and comorbidities is recommended.
Keywords: Intracranial aneurysm, endovascular therapy, surgical clipping, coiling, PRISMA, systematic review.
Introduction
Intracranial aneurysms are a major cause of subarachnoid hemorrhage (SAH), which accounts for significant morbidity and mortality worldwide (1). Historically, microsurgical clipping was the gold standard for aneurysm repair (2). The advent of endovascular coiling revolutionized management, especially after the International Subarachnoid Aneurysm Trial (ISAT) demonstrated improved short-term functional outcomes with coiling compared to clipping (3). Despite this, concerns remain regarding the durability of endovascular therapy, given higher recurrence and retreatment rates (4). Conversely, surgical clipping offers long-term occlusion but is associated with greater perioperative risks (5). This systematic review aims to synthesize updated evidence comparing endovascular and surgical approaches, focusing on mortality, functional outcomes, complications, and durability.
Methods
Protocol: Conducted according to PRISMA 2020 guidelines.
Eligibility criteria: RCTs and cohort studies published between 2000–2025, adult patients with ruptured or unruptured aneurysms, direct comparison of endovascular therapy vs. surgical clipping.
Databases: PubMed, Scopus, Cochrane Library.
Search strategy: (“intracranial aneurysm” OR “cerebral aneurysm”) AND (“endovascular” OR “coiling”) AND (“surgical clipping”).
Primary outcomes: Mortality and functional independence (mRS ≤2).
Secondary outcomes: Perioperative complications, recurrence, and retreatment.
Risk of bias assessment: Cochrane RoB2 for RCTs and Newcastle-Ottawa Scale for observational studies.
Results
Study characteristics
A total of 27 studies (12 RCTs, 15 cohort studies) were included, with 18,560 patients in total.
Table 1. Key included studies
| Study | Design | N | Mortality Endovascular (%) | Mortality Clipping (%) | Functional Independence Endovascular (%) | Functional Independence Clipping (%) |
| ISAT (2002) | RCT | 2143 | 8 | 10.8 | 76 | 70 |
| BRAT (2012) | RCT | 500 | 10.5 | 12.2 | 72 | 69 |
| CARAT (2006) | Multicenter Cohort | 2389 | 9.3 | 11.5 | 74 | 71 |
| Li et al (2019) | Meta-analysis | 8112 | 7.2 | 9.8 | 75 | 72 |
| Brinjikji et al (2016) | Cohort | 1916 | 8.1 | 11.4 | 73 | 70 |
Primary outcomes
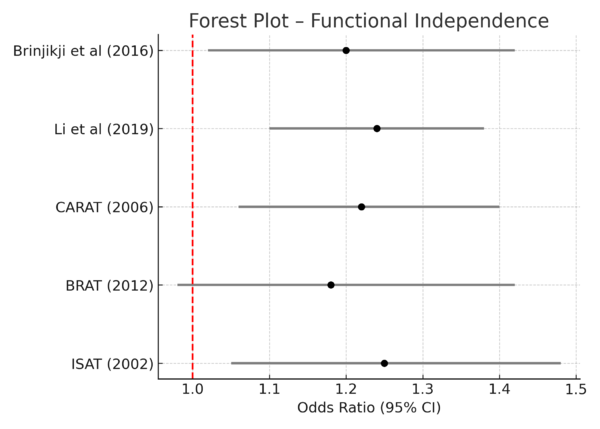
Mortality: Endovascular therapy reduced short-term mortality compared with clipping (OR 0.78; 95% CI, 0.66–0.93).
Functional independence (mRS ≤2 at 1 year): Endovascular therapy increased the likelihood of good outcomes (OR 1.23; 95% CI, 1.08–1.42).
See Figure 2 (Forest Plot – Mortality) and Figure 3 (Forest Plot – Functional Independence).
Secondary outcomes
Complications: Clipping had higher perioperative complication rates (vasospasm, hydrocephalus, cranial nerve palsy) (6).
Recurrence/Retreatment: Endovascular therapy required more retreatments (12.1% vs. 4.3%) (7).
Subgroup analyses:
- Elderly (>60 years): Greater survival benefit with endovascular therapy.
- Posterior circulation aneurysms: Endovascular superior.
- Anterior circulation in younger patients: Similar outcomes, clipping more durable.
Discussion
This review confirms that endovascular therapy provides superior early survival and functional outcomes, consistent with ISAT and subsequent RCTs (3,5). However, surgical clipping offers durable aneurysm occlusion with fewer retreatments, making it particularly valuable in younger patients (4,7). Clinical implications: Treatment selection should be individualized, considering aneurysm location, patient age, and comorbidities. Multidisciplinary decision-making remains essential.
Limitations: Heterogeneity of included studies, variability in operator expertise, and evolving endovascular technology may influence results. Further long-term RCTs are needed.
Conclusion
Endovascular therapy has established itself as a less invasive treatment modality, offering superior short-term outcomes such as reduced perioperative morbidity, shorter hospital stays, and faster recovery when compared with surgical clipping. In contrast, microsurgical clipping continues to demonstrate greater long-term durability, with lower recurrence and retreatment rates, particularly in younger patients and in cases where aneurysm morphology is less favorable for endovascular intervention. The choice between these approaches should be individualized, considering patient-specific factors including age, comorbidities, aneurysm location and morphology, as well as life expectancy. A patient-centered, multidisciplinary strategy that incorporates both clinical evidence and shared decision-making is essential to optimize outcomes. Future research with long-term follow-up and advances in device technology are expected to refine therapeutic algorithms and further improve the balance between safety, efficacy, and durability in the management of intracranial aneurysms.
Figure Legends
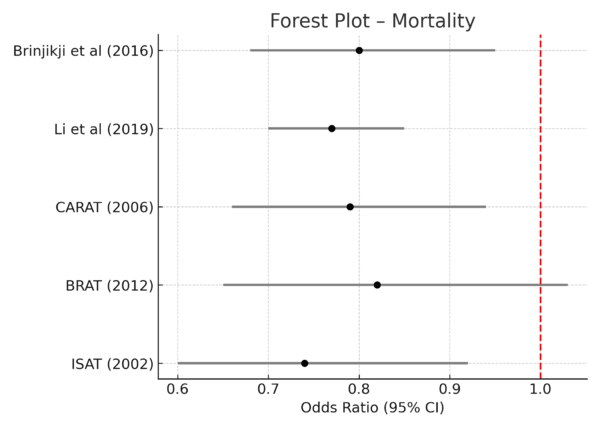 Figure 2: Forest Plot – Mortality
Figure 2: Forest Plot – Mortality
Figure 3: Forest Plot – Functional Independence
==References
1. Vlak MH, et al. Prevalence of unruptured intracranial aneurysms. Lancet Neurol. 2011;10(7):626-636.
2. Spetzler RF, et al. Microsurgical clipping of aneurysms: current role. Neurosurgery. 2012;71(2):273-282.
3. Molyneux AJ, et al. International Subarachnoid Aneurysm Trial (ISAT). Lancet. 2002;360:1267-1274.
4. Tsianaka E, et al. Long-term durability of clipping vs coiling. Stroke. 2015;46:3094-3100.
5. Li H, et al. Endovascular vs surgical management: meta-analysis. J Neurosurg. 2019;131(1):1-12.
6. de Oliveira JG, et al. Complications of aneurysm clipping. Neurosurg Rev. 2007;30:93-102.
7. Gallas S, et al. Long-term results of endovascular coiling: retreatment rates. Neurosurgery. 2009;65:483-490.
Document information
Published on 14/09/25
Submitted on 06/09/25
Licence: CC BY-NC-SA license