Summary
Advanced hepatocellular carcinoma has a poor therapeutic outcome and treatment options are limited. Sorafenib, an orally active multikinase inhibitor, is the only systemic drug that has been shown to provide survival benefits in randomized control studies. However, the gains in survival are modest and new treatment strategies are needed. We report here the case of a patient with advanced hepatocellular carcinoma who had an impressive response to a combination of sorafenib and radiotherapy. The treatment was well tolerated with no unexpected toxicities. Post-treatment imaging showed a satisfactory partial response with regression of the tumor by more than 50%.
Keywords
Hepatocellular carcinoma ; Sorafenib ; Radiotherapy
Introduction
Hepatocellular carcinoma (HCC) is the fifth most common cancer and the third cause of cancer-related death in the world (responsible for one million deaths per year) [1] . In Taiwan, HCC is the leading cause of cancer death, with approximately 8000 new cases diagnosed and 7000 deaths occurring annually. The 5-year survival rate of patients with HCC is less than 10%, even with aggressive conventional treatment. The treatment options for HCC are either curative or palliative. Curative treatments, which achieve the best outcomes, include liver resection and transplantation, whereas palliative treatments include tumor ablation, embolization, radiotherapy, and chemotherapy [2] . When aggressive treatments fail, there is currently no effective salvage treatment available. Clinical trials of multikinase inhibitors, such as sorafenib, have given impressive results, with a moderate improvement in survival for advanced HCC in patients with Child–Pugh grade A cirrhosis [3] . However, there are limited options for the management of HCC in patients with Child–Pugh grade B cirrhosis. We report here the case of a 68-year-old man with advanced HCC related to hepatitis C and Child–Pugh grade B cirrhosis. This patient was successfully treated with sorafenib combined with radiotherapy.
Case report
A 63-year-old Chinese man with a history of chronic hepatitis C without regular follow up presented to our emergency department with right upper quadrant abdominal pain and general weakness. A physical examination showed hepatosplenomegaly with abdominal tenderness and an abdominal ultrasound scan showed liver cirrhosis with suspected liver tumors. He was admitted to our gastrointestinal ward on November 3, 2010 for further management. His α-fetoprotein level was elevated (1032 ng/ml); however, his liver profile was Child–Pugh grade B. Imaging studies (abdominal magnetic resonance imaging) showed multiple T1W1-low and T2W1-high intensity lesions of variable sizes with early contrast enhancement over the whole liver except for segments 1 and 5, and extensive tumor thrombus involving the portal venous system, both hepatic veins, and extending into the inferior vena cava. HCC was diagnosed on the basis of his hepatitis C status with typical radiological findings and raised serum α-fetoprotein level. He had a European Cooperative Oncology Group performance status 1, a Barcelona Clinic Liver Cancer (BCLC) [4] classification stage C, and Cancer of the Liver Italian Program score 2. He was given Duragesic (fentanyl transdermal) for a short period to control his pain. Chemoembolization was not offered due to the extensive macrovascular involvement.
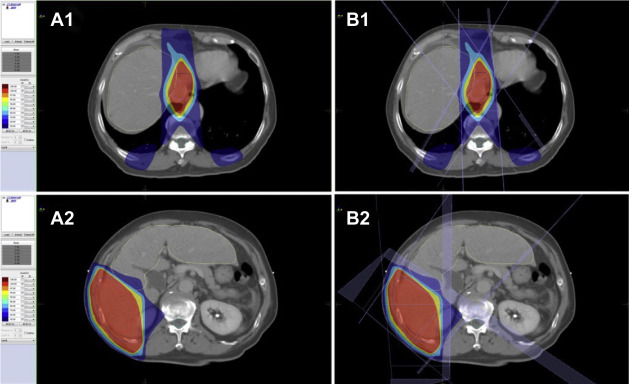
Palliative radiation therapy (three-dimensional conformal radiotherapy) was given 5 days per week at 1.8 Gy per day to the portal vein and tumor of the right lobe for 28 fractions to a total dose of 50.4 Gy; treatment with sorafenib (400 mg per day) was started on December 10, 2010. Fig. 1 A1,B1 and A2,B2 shows the dose distribution for the tumor, portal vein, and surrounding organs and tissues.
|
|
|
Figure 1. Computed tomography scans of our patient with hepatocellular carcinoma showing dose distribution of radiation from proton beam therapy (A) and that from standard X-rays using the same beam arrangement (B). The 100%, 95%, 80%, and 50% isodose lines are represented in red, yellow, light blue, and dark blue, respectively. The planning target volume (PTV) is represented in pink. The protocol required the PTV to be encompassed by the 95% dose envelope. (A1), (B1) On liver tumor. (A2), (B2) On portal vein. GTV = gross tumor volume. |
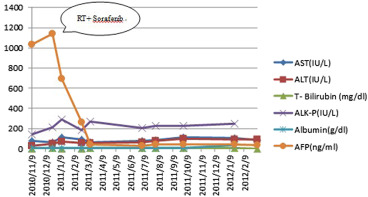
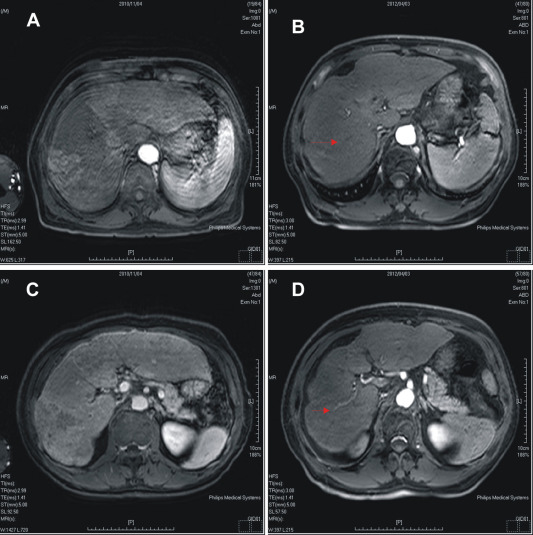
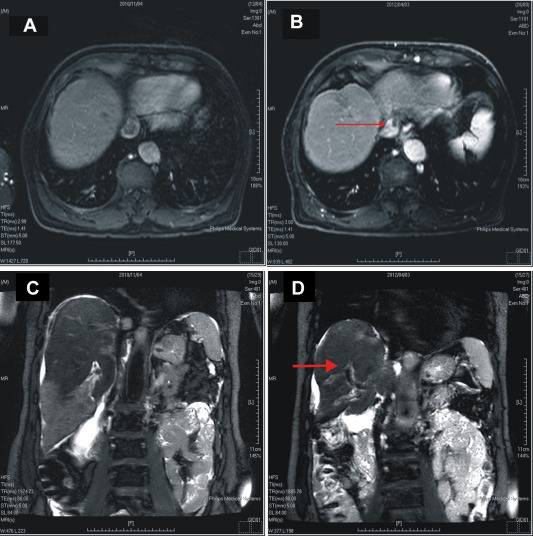
The patients symptoms improved gradually with no abdominal pain and his appetite improved. The follow-up examination 6 months later indicated an early response, with a dramatic reduction in the size of the liver masses (8 cm to 3 cm) and a decrease in the α-fetoprotein level. He experienced manageable side-effects of mild diarrhea, itching of the skin with red papules over his scalp, Grade 2–3 hand and foot skin reactions, lesser control of hypertension, and some hair loss. On completion of 16 months of treatment he had ongoing marked clinical, radiological, and biochemical responses (Figure 2 , Figure 3 ; Figure 4 ).
|
|
|
Figure 2. Changes in laboratory data over time after treatment with sorafenib and radiotherapy. AFP = α-fetoprotein; ALK-P = serum alkaline phosphatase; ALT = serum alanine aminotransferase; AST = serum aspartate aminotransferase; T-Bilirubin = total bilirubin. |
|
|
|
Figure 3. Effect of treatment with sorafenib and radiotherapy evaluated by abdominal magnetic resonance imaging. (A), (B) Pretreatment and post-treatment in arterial phase. Part (B) also shows decreased tumor size in arterial phase after treatment (arrow); (C), (D) pretreatment and post-treatment in delayed phase. Part (D) also shows decreased tumor thrombus in the portal vein after treatment (arrowhead). |
|
|
|
Figure 4. Effect of treatment with sorafenib and radiotherapy evaluated by abdominal magnetic resonance imaging. (A) Tumor thrombus in the inferior vena cava before treatment in delayed phase; (B) decreased tumor thrombus in the inferior vena cava after treatment (arrow); (C) tumor thrombus in the portal vein before treatment in coronal view; and (D) decreased tumor thrombus in the portal vein after treatment (arrow). |
Discussion
Sorafenib is an orally active multikinase inhibitor that has been shown to affect tumor cell proliferation and tumor angiogenesis. It inhibits molecular components of the Raf–MEK–ERK signaling pathway, abrogating tumor growth and vascular endothelial growth factor receptors (VEGFR) 1, 2 and 3, and endothelial growth factor receptors PDGFR-β, thus inhibiting neoangiogenesis [5] . Sorafenib emerged as the first effective systemic treatment in HCC after 30 years of research and is currently the standard of care for patients with advanced tumors. Following an initial Phase II study showing a signal of efficacy [3] , a large double-blinded placebo-controlled Phase III investigation was conducted, leading to positive survival results. In this trial, the benefit of sorafenib was to increase the median overall survival time from 7.9 months in the placebo group to 10.7 months in the sorafenib group (hazard ratio = 0.69; 95% confidence interval 0.55–0.87; p = 0.00058), which represents a 31% decrease in the relative risk of death.
The panel of experts recommends using sorafenib as the standard systemic treatment for HCC. It is indicated for patients with well-preserved liver function (Child–Pugh class A) and with advanced tumors of BCLC class C [6] . No clear recommendation can be made in patients of Child–Pugh class B liver function. Sorafenib is currently being tested in the adjuvant setting after resection or complete local ablation for early stage disease, in combination with chemoembolization for intermediate stages [7] , in combination with erlotinib or systemic doxorubicin in advanced stages, and as a first-line treatment in Child–Pugh B class patients.
Historically, radiotherapy has always played a limited part in the treatment of HCC as a result of a lack of high evidence level data, especially randomized controlled trials. The low tolerance of the liver and the subsequent risk of radiation-induced liver disease have posed obstacles to including radiotherapy in the routine treatment of HCC [8] . However, radiotherapy has undergone major technological improvements over the last few decades, including diagnostic imaging, radiotherapy planning techniques (three-dimensional conformal radiotherapy, intensity-modulated radiotherapy, and stereotactic body radiosurgery), and image-guided radiotherapy to detect to the exact position of the tumor at the time of treatment so that higher doses can be targeted to the tumor while minimizing exposure to normal liver tissue. The evidence supporting radiotherapy as a safe and efficacious option for the treatment of HCC continues to grow and is summarized in Table 1[9] . Radiotherapy is now an important option in patients with unresectable HCC or with portal vein thrombosis [8] .
| Reference | n | Child–Pugh A and B (%)a | Tumor size | Total dose (Gy) (number fraction) | Response (%) | 2-yr LC (%) | 1-yr OS (%) | 2-yr OS (%) | 3-yr OS (%) | 5-yr OS (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Mornex et al (2006); (Phase II) | 25 | A 64 (16/25) B 44 (11/25) | 1 nodule <5 cm; 2 nodules <3 cm | 66 (2 y/fx × 30) | 92; CR 80; PR 12 | |||||
| Kim et al (2005) | 59 35 (s/p RFA TACE) | PVT (+) | 30–54 | 45.8 | 40.7 | 20.7 | ||||
| Seong et al (R) (2003) | 158 | A 74; B 26 | 51% PVT(+) 49% PVT(–) 75% <10 cm 25% >10 cm | 67.1 | 59.4 | 30.5 | 9 | |||
| Liu et al (2004) | 44 | A 72 (32/44); B 27 (12/44) | 6–25 cm | 40–60 | 61; CR 13; PR 25–78 | 60.5 | 40.3 | 32 | 9–19 | |
| Bush et al (2004) (Phase II) | 37 | 5.6 cm (1.5–10 cm) | 42 (×15 fx) | 75 | 55 |
CR = complete response; fx = fractions; LC = local control; OS = overall survival; PR = partial response; PVT = Portal vein thrombosis; R = retrospective; RFA = Radiofrequency ablation; SD = stable disease; s/p = status post; TACE = Transarterial chemoembolization.
Note. From “Radiotherapy and hepatocellular carcinoma: update and review of the literature,” by S. Ursino, C. Greco, F. Cartei, C. Colosimo, A. Stefanelli, B. Cacopardo, et al, 2012, Eur Rev Med Pharmacol Sci 16 , pp. 1599–604. Copyright 2012, European Review for Medical and Pharmacological Sciences. Adapted with permission.
a. Child–Pugh B score patients are more likely to develop radiation-induced liver disease.
Preclinical studies have documented improved outcomes through synergistic antitumor activity with the combination of VEGF or VEGFR inhibitors and irradiation, with the combination resulting in a longer delay in tumor growth and higher local tumor control than either treatment alone [8] . The mechanisms underlying the additive effect of these modalities are complex and include decreased tumor hypoxia and the radiosensitization of endothelial cells. Antiangiogenic drugs result in a relative normalization of blood flow in tumors, with a more efficient delivery of oxygen and therapeutic agents to the targeted malignant cells. Therefore increasing the oxygenation of tumors would be expected to improve their radiation response. However, evidence for the clinical use of this combined treatment in patients with HCC is lacking. Our patient tolerated the combined regimen well, with a reduction in tumor volume of more than 75%, reduced tumor thrombus in the portal, hepatic, and inferior vena cava, and a decrease in α-fetoprotein level of 97% after treatment. According to the response evaluation criteria [10] in solid tumors guidelines, post-treatment imaging showed a partial response with regression of the tumor by more than 50%.
In conclusion, improved outcomes have been shown with sorafenib and radiotherapy for the treatment of advanced HCC, as seen in the case reported here. Further studies addressing the combination of these modalities are warranted to confirm the efficacy, toxicity, and optimal sequencing of this treatment.
Conflicts of interest
All contributing authors declare no conflicts of interest.
References
- [1] F.X. Bosch, J. Ribes, M. Díaz, R. Cléries; Primary liver cancer: worldwide incidence and trends; Gastroenterology, 127 (2004), pp. S5–16
- [2] J. Bruix, M. Sherman; Management of hepatocellular carcinoma; Hepatology, 42 (2005), pp. 1208–1236
- [3] G.K. Abou-Alfa, L. Schwartz, S. Ricci, D. Amadori, A. Santoro, A. Figer, et al.; Phase II study of sorafenib in patients with advanced hepatocellular carcinoma; J Clin Oncol, 24 (2006), pp. 4293–4300
- [4] J.M. Llovet, C. Bru, J. Bruix; Prognosis of hepatocellular carcinoma: the BCLC staging classification; Semin Liver Dis, 19 (1999), pp. 329–338
- [5] J.A. Gollob, S. Wilhelm, C. Carter, S.L. Kelley; Role of Raf kinase in cancer: therapeutic potential of targeting the Raf/MEK/ERK signal transduction pathway; Semin Oncol, 33 (2006), pp. 392–406
- [6] J.M. Llovet, S. Ricci, V. Mazzaferro, P. Hilgard, E. Gane, J.F. Blanc, et al.; Sorafenib in advanced hepatocellular carcinoma; N Engl J Med, 359 (2008), pp. 378–390
- [7] T.H. Kim, D.Y. Kim, J.W. Park, Y.I. Kim, S.H. Kim, H.S. Park, et al.; Three-dimensional conformal radiotherapy of unresectable hepatocellular carcinoma patients for whom transcatheter arterial chemoembolization was ineffective or unsuitable; Am J Clin Oncol, 29 (2006), pp. 568–575
- [8] B.B. Ma, R.G. Bristow, J. Kim, L.L. Siu; Combined-modality treatment of solid tumors using radiotherapy and molecular targeted agents; J Clin Oncol, 21 (2003), pp. 2760–2776
- [9] S. Ursino, C. Greco, F. Cartei, C. Colosimo, A. Stefanelli, B. Cacopardo, et al.; Radiotherapy and hepatocellular carcinoma: update and review of the literature; Eur Rev Med Pharmacol Sci, 16 (2012), pp. 1599–1604
- [10] E.A. Eisenhauer, P. Therasse, J. Bogaerts, L.H. Schwartz, D. Sargent, R. Ford, et al.; New response evaluation criteria in solid tumours: Revised RECIST guideline; European Journal of Cancer, 45 (2009), pp. 228–247
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?