Summary
A 1-year-old boy with no underlying disorder presented with non-bilious vomiting since 4 days before admission. He was referred to our hospital and was diagnosed with a small bowel obstruction due to an intraabdominal tumor. Laparotomy revealed an intestinal volvulus with a soft and lobulated tumor arising from the mesentery. The resected tumor with a small part of the small bowel was diagnosed as lipoblastoma histologically. From a literature review, mesenteric lipoblastoma with an intestinal volvulus showed different characteristics such as greater frequency of vomiting and less frequency of abdominal mass as clinical symptoms, and the size of the tumor was smaller than that of the tumor without the intestinal volvulus.
Keywords
lipoblastoma;mesenterium;volvulus
1. Introduction
Lipoblastoma is a benign soft tissue tumor originating from embryonal white fat tissue. Most cases are found in infants and young children, especially in the age of 3 years or younger.1 ; 2 The tumor frequently occurs in the subcutaneous tissues of the extremities and the trunk.3; 4 ; 5 It can also arise in the retroperitoneum, abdomen, chest, mediastinum, scrotum, and so on.6; 7 ; 8 Among these, mesenteric occurrence is rare, and only 19 cases have been reported to date. In this report, we present an additional case of mesenteric lipoblastoma developing into a small intestinal volvulus and also review the reported cases with mesenteric lipoblastoma.
2. Case report
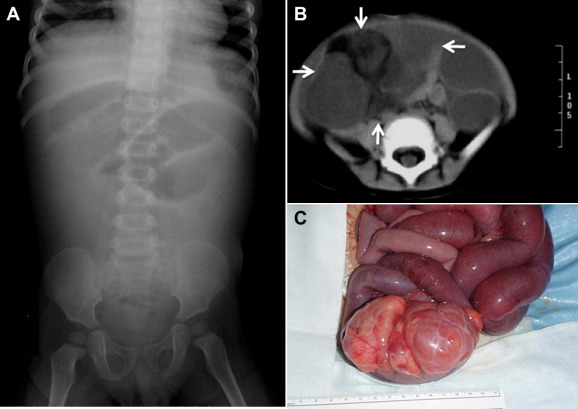
A 1-year-old boy with no underlying disorder presented with nonbilious vomiting since 4 days before admission. He visited a hospital because the vomiting has been getting bilious and more frequent with abdominal distension. Imaging tests showed small intestinal obstruction due to the mass lesion, and he was referred to our hospital to further intervention. On admission, he looked pale and lifeless. On palpation, the abdomen was markedly distended without peritoneal signs and an elastic, soft, and mobile mass was detected in the right lower abdomen with a measurement of 10 cm × 5 cm. Laboratory investigations revealed mild anemia, hyponatremia, and hypochloremia without other remarks. Abdominal X-ray film showed small bowel obstruction (SBO) (Fig. 1A). Abdominal computerized tomography (CT) scan revealed dilated small bowel and a heterogeneous mass without calcification (Fig. 1B). Patient underwent an emergent laparotomy with a preoperative diagnosis of SBO due to an intraabdominal tumor containing fat tissues. On operation, it was noticed that a soft and lobulated tumor with a smooth, glistening capsule arose from the mesentery of ileum, and small intestine was rotated 360° around the tumor (Fig. 1C). An additional 360° rotated small intestinal volvulus around the proximal mesentery was also found. Although there was no sign of necrosis in the small intestine, the tumor severely adhered to the border of the small intestines, and it was difficult to remove the tumor without bowel resection. We resected the tumor en bloc, including the small bowel, which was 15 cm in length. Histological findings were compatible with those of lipoblastoma without evidence of tumor invasion to the bordering intestine. The postoperative course was uneventful, and he was discharged from the hospital on postoperative day 10. There is no evidence of recurrence on clinical symptom and magnetic resonance imaging (MRI) examination for 1 year after operation.
|
|
|
Figure 1. (A) Abdominal plain X-ray demonstrated small bowel obstruction. (B) Abdominal computed tomography revealed dilated small bowel and a heterogeneous mass without calcification. (C) Intraoperative photograph shows a soft and lobulated tumor with smooth, glistening capsule arising from the mesentery 180 cm distal to the Treitz' ligament. It shows that the small intestine has rotated 360° around the tumor, and an additional 360° rotated small intestinal volvulus around the more proximal mesentery was also found. |
3. Discussion
The lipoblastoma is rare, benign tumor composed of fetal adipose tissue.9 Most of them are seen in infants and young children, and 80-90% of cases occur at 3 years of age or younger.1 ; 2 Boys are affected two to three times more often than girls.10 Lipoblastoma is commonly located in the extremities3; 4 ; 5 and also in the body trunk, head and neck, mediastinum, inguinal region, scrotum, buttock, perirectal area, retroperitoneum, and rarely the mesentery.6; 7 ; 8
Abdominal lipoblastomas represent roughly 7% of all lipoblastomas, and most lipoblastomas arise in the retroperitoneum.3; 4 ; 11 Among 24 studies that reported the cases arising in the mesentery, 18 cases were described in detail.9; 12; 13; 14; 15; 16; 17; 18; 19; 20; 21; 22; 23; 24; 25 ; 26 Then, we reviewed 19 cases, including our additional case in this study, and investigated whether the clinical difference in mesenteric lipoblastoma complicated the intestinal volvulus or not (Table 1). Statistical analysis was performed using Statview 5.0 for Windows (SAS Institute Inc., Cary, NC). Values for continuous variables were expressed as mean ± 1 standard deviation. The Mann-Whitney U test and Fishers exact Chi-square test were used to compare the observed differences between the groups; p < 0.05 was considered statistically significant.
| Volvulus group (n = 3) | Nonvolvulus group (n = 14) | p value | |
|---|---|---|---|
| Gender (boy/girl) | 2/1 | 9/5 | n.s. |
| Age (mean ± SD, year) | 3.3 ± 3.2 | 2.0 ± 1.2 | n.s. |
| Symptoms at presentation to hospital | |||
| Abdominal mass or distension | 0 (0%) | 10 (71%) | p = 0.025 |
| Abdominal pain | 1 (33%) | 4 (29%) | n.s. |
| Vomiting | 3 (100%) | 2 (14%) | p = 0.0031 |
| Location | |||
| Jejunum | 2 (66%) | 2 (14%) | n.s. |
| Ileum | 1 (33%) | 5 (36%) | |
| Transverse colon | 0 (0%) | 1 (7%) | |
| Unknown | 0 (0%) | 6 (43%) | |
| Maximum diameter of the tumor (mean ± SD, range, cm) | 9.7 ± 1.5, 8–11 | 15.3 ± 3.6, 9.7–23 | p = 0.024 |
| Intestinal resection (yes/no) | 2/1 | 6/8 | n.s. |
n.s.: not significant.
A small intestinal volvulus was found in three cases, including our present case9 ; 14; however, there is no case associated with intestinal necrosis. There was no difference in gender and age at onset between the volvulus and nonvolvulus groups. Considering the patients' symptoms on visiting the hospital, patients in the volvulus group revealed an abdominal mass less frequently and vomiting more frequently than those in the nonvolvulus group, which were statistically significant (p = 0.035 and 0.0055, respectively). There was no difference in the location of the tumor between both groups. The diameter of the lipoblastoma in the volvulus group was significantly smaller than that of the lipoblastoma in the nonvolvulus group (8.8 ± 1.0 cm, 8–10 in range vs. 15.4 ± 3.3 cm, 11–23 in range, p = 0.0094). Although the lipoblastoma is a benign tumor and only complete tumor resection is the effective procedure, 9 out of 19 (47%) cases needed additional bowel resection because of severe tumor adhesion to the border of the intestine such as in the present case. There is no difference in intestinal resection rate between the volvulus and nonvolvulus groups. No recurrence cases have been reported in the mesenteric lipoblastoma to date in the literature.
Lipoblastoma arising from the mesentery is extremely rare, and cure is expected by complete resection of a tumor with or without a part of the intestine. Mesenteric lipoblastoma with an intestinal volvulus had different characteristics such as more frequency of vomiting and less frequency of abdominal mass as clinical symptoms and the size of the tumor was smaller than that of the tumor without the intestinal volvulus.
References
- 1 E.B. Chung, F.M. Enzinger; Benign lipoblastomatosis: an analysis of 35 cases; Cancer, 32 (1973), pp. 482–491
- 2 C.M. Coffin; Lipoblastoma: an embryonal tumor of soft tissue related to organogenesis; Semin Diagn Pathol, 11 (1994), pp. 98–103
- 3 I.S. Arda, M.E. Senocak, S. Gogus, N. Buyukpamukcu; A case of benign intrascrotal lipoblastoma clinically mimicking testicular torsion and review of the literature; J Pediatr Surg, 28 (1993), pp. 259–261
- 4 A.V. Dilley, D.L. Patel, M.J. Hicks, M.L. Brandt; Lipoblastoma: pathophysiology and surgical management; J Pediatr Surg, 36 (2001), pp. 229–231
- 5 T. Mentzel, E. Calonje, C.D.M. Fletcher; Lipoblastoma and lipoblastomatosis: a clinicopathological study of 14 cases; Histopathology, 23 (1993), pp. 527–533
- 6 Y.S. Chun, W.K. Kim, K.W. Park, S.C. Lee, S.E. Jung; Lipoblastoma; J Pediatr Surg, 36 (2001), pp. 905–907
- 7 S.M. Jung, P.Y. Chang, C.C. Luo, C.S. Huang, J.Y. Lai, C. Hsueh; Lipoblastoma/lipoblastomatosis: a clinicopathologic study of 16 cases in Taiwan; Pediatr Surg Int, 21 (2005), pp. 809–812
- 8 A.L. Speer, D.E. Schofield, K.S. Wang, et al.; Contemporary management of lipoblastoma; J Pediatr Surg, 32 (1997), pp. 1771–1772
- 9 A.H. Al-Salem, M. Al-Nazer; Mesenteric lipoblastoma in a 2-year-old child; Pediatr Surg Int, 19 (2003), pp. 115–117
- 10 T. Reiseter, T. Nordshus, A. Borthne, B. Roald, P. Naess, O. Schistad; Lipoblastoma: MRI appearances of a rare paediatric soft tissue tumor; Pediatr Radiol, 29 (1999), pp. 542–545
- 11 M.R. McVay, J.E. Keller, C.W. Wagner, R.J. Jackson, S.D. Smith; Surgical management of lipoblastoma; J Pediatr Surg, 41 (2006), pp. 1067–1071
- 12 H.M. Jia, K.R. Zhang; Mesenteric lipoblastoma in a 4-year-old; Pediatr Radiol, 39 (2009), p. 1126
- 13 X.B. Tang, T. Zhang, Y.Z. Bai, W.L. Wang; Giant mesenteric lipoblastoma in a 4-year-old child; J Pediatr Surg, 44 (2009), pp. 859–861
- 14 D.C. Yu, P.J. Javid, K.R. Chikwava, et al.; Mesenteric lipoblastoma presenting as a segmental volvulus; J Pediatr Surg, 44 (2009), pp. e25–e28
- 15 R. Cudnik, P.A. Efron, M.K. Chen, J.D. Reith, E.A. Beierle; Mesenteric lipoblastoma: a rare location in children; J Pediatr Surg, 43 (2008), pp. e5–e7
- 16 Y.H. Mo, S.S. Peng, Y.W. Li, C.T. Shun; Mesenteric lipoblastoma: case report; Pediatr Radiol, 33 (2003), pp. 37–40
- 17 K.A. O'Donnell, M.G. Caty, J.E. Allen, J.E. Fisher; Lipoblastoma: better termed infantile lipoma?; Pediatr Surg Int, 16 (2000), pp. 458–461
- 18 Y. Posey, E. Valdivia, D.L. Persons, et al.; Lipoblastoma presenting as a mesenteric mass in an infant; J Pediatr Hematol Oncol, 20 (1998), pp. 580–582
- 19 M.M. Beebe, M.D. Smith; Omental lipoblastoma; J Pediatr Surg, 18 (1993), pp. 1626–1627
- 20 H. Schulman, Y. Barki, Y. Hertzanu; Case report: mesenteric lipoblastoma; Clin Radiol, 46 (1992), pp. 57–58
- 21 A. Prando, S. Wallace, J.L. Marins, R.M. Pereira, E.R. de Oliveira, M. Alvarenga; Sonographic features of benign intraperitoneal lipomatous tumors in children–report of 4 cases; Pediatr Radiol, 20 (1990), pp. 571–574
- 22 G. Zanetti; Benign lipoblastoma: first case report of a mesenteric origin; Tumori, 74 (1988), pp. 495–498
- 23 F.M. Denath; Case of the season; Semin Roentgenol, 23 (1988), pp. 241–242
- 24 J.F. Jimenez; Lipoblastoma in infancy and childhood; J Surg Oncol, 32 (1986), pp. 238–244
- 25 G. Stringel, B. Shandling, K. Mancer, S.H. Ein; Lipoblastoma in infants and children; J Pediatr Surg, 17 (1982), pp. 227–280
- 26 A.L. Speer, D.E. Schofield, K.S. Wang, et al.; Contemporary management of lipoblastoma; J Pediatr Surg, 43 (2008), pp. 1295–1300
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?