Summary
Objective
There is controversy concerning the management of the remaining cavity after the evacuation of a cyst in patients who have undergone surgical operation for liver hydatidosis. This study compares the results of capitonnage and tube drainage of the remaining cavity.
Methods
In this retrospective study, participants were selected from two groups of patients with a liver hydatid cyst who underwent capitonnage or tube drainage from 2004 to 2012. The patients were followed for 6–24 months. The data of age, sex, involved liver lobe, size of the cyst, complications, drain duration, and hospital stay were analyzed.
Results
Participants included 155 patients consisting of 96 (61.94%) females and 59 (38.06%) males. Most cysts were in the right lobe, and the most common diameter of the cysts was greater than 10 cm. Capitonnage was performed on 90 (58.06%) patients and the tube drainage procedure was performed on the remaining 65 (41.94%) patients. In the tube drainage group and the capitonnage group, the operative times were 2.21 ± 0.65 hours and 2.53 ± 0.35 hours, respectively; the hospital stays were 5.695 ± 3.37 days and 4.43 ± 2.96 days, respectively; the drain duration was 9.2 ± 1.7 days and 2.1 ± 0.4 days, respectively; and the time to return to work was 14.7 ± 2.3 days and 8.3 ± 10.4 days, respectively. All variables were statistically significant, except for the operative time. Cavity infection and biliary fistula were identified in three patients and six patients, respectively, in the tube drainage group and identified in two patients and three patients, respectively, in the capitonnage group. This difference was not statistically significant.
Conclusion
This study demonstrated that capitonnage versus the tube drainage method may result in a shorter hospital stay, decreased time to return to work, and low rate of morbidity and complications.
Keywords
capitonnage;liver hydatid cyst;tube drainage
1. Introduction
Hydatid cyst is a parasitic disease caused by the tapeworm Echinococcus granulosus or Echinococcus alveolaris. The prevalence of the disease varies around the world. Hydatid disease is encountered in specific areas such as Mediterranean countries, Australia and New Zealand, South America and Central America, the Middle East, India, and China. 1 ; 2 Common locations of the parasitic infection are the liver (60–70%) and lungs (30%), whereas cysts are rarely in the kidney, pericardium, brain, bones, and muscles. 3 ; 4 With regard to disappointing medical therapy of hydatid disease, surgery has long been considered the mainstay in the treatment of this disease. A variety of surgical techniques has been proposed for the involved liver. These include open approaches such as pericystectomy, hepatic resection, and drainage or obliteration of the cavity (which can potentially be performed laparoscopically). Minimally invasive techniques such as the percutaneous aspiration infusion re-aspiration technique (PAIR: Puncture, aspiration, injection, re-aspiration) have also been developed. 5 ; 6 Bülbüller et al7 concluded that there is no significant difference in the rates of complications and recurrences among the different surgical procedures if they are performed with basic rules of surgical principles. Some surgeons believe that, in benign disease of the liver, complete resection is time-consuming and unnecessary; other surgeons have argued that resection may increase the operative risk because of vascular and biliary injuries but, because of lower postoperative recurrence and morbidity, it can be performed on multiple cysts that are adjacent to each other or close to a major blood supply, or performed on cysts in a safe location.6 Balik et al8 indicate that capitonnage, omentoplasty, cyst excision, segmentectomy, or cystoenterostomy are all superior to tube drainage for managing hydatid disease of the liver. Filippou et al5 performed a modified capitonnage technique in partial cystectomy, which led to a fast and effective mobilization of the patients and reduction of postoperative bile leakage.5 Voros et al9 demonstrated that the selection of appropriate patients and use of interdisciplinary treatment approaches, and a surgeons experience are the most important factors for attaining the best results in the management of these patients. This study aimed to compare the results and the complications of two surgical methods: capitonnage and tube drainage of the remaining cavity after evacuation of the cyst in patients with liver hydatid cyst.
2. Patients and methods
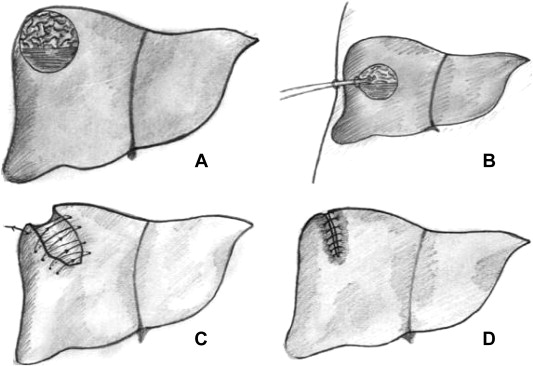
The medical records of 155 patients treated for hydatid disease from 2004 to 2012 in our institution were reviewed retrospectively. Of these patients, 59 (38.06%) were male and 96 (61.94%) were female. Their preoperative diagnosis was established by history, clinical examination, ultrasonography (US) scanning, and computed tomography (CT) scanning. All patients underwent chest radiography. The treatment for all patients was surgery. All patients received albendazole (10 mg/kg of body weight) preoperatively for 1 month. In all patients, after the abdominal cavity had been isolated with a compressed abdominal pad soaked in 15% hypertonic saline solution, the cyst was punctured and the hydatid fluid was aspirated to reduce the pressure within the cyst. The cyst was then widely opened by excising the projecting part of the pericyst and evacuating its contents. The remaining cavity was irrigated with sterile hypertonic saline. The cavities were explored for possible cystobiliary communication. Treatment consisted of closure of the communications using fine absorbable 0 Vicryl sutures (Supa. Co. Ltd, Tehran, Iran). In the tube drainage group, external drainage of the residual cavity was performed using a wide-gauge rubber tube pursed by the remaining cystic wall. A drain was applied through a stab wound and connected with a bag for gravity drainage. The suprahepatic and subhepatic spaces were also drained in all patients. Tubes were removed within a few days in the absence of bile leakage or any discharge (Fig. 1A and B). In the second group, the capitonnage procedure was performed to obliterate the remaining cavity. In this procedure, the remaining walls of the cavity are anchored to the posterior wall by a series of purse-string sutures or mattress sutures (Fig. 1C and D). Capitonnage was not possible when the cyst was large or the cavity walls were calcified and rigid. In our series, capitonnage was performed on 90 (58.06%) patients and tube drainage was performed in 65 (41.94%) patients. Coexistent cysts were treated by splenectomy and cyst excision. For lung cysts, thoracotomy was primarily performed.
|
|
|
Figure 1. The schematic figure of tube drainage versus capitonnage. (A) The primary cyst. (B) Tube drainage of the remaining cavity. (C) Anchoring the remaining walls of the cavity to the posterior wall in capitonnage. (D) The remaining cavity after capitonnage. |
Statistical analyses were performed using the Student t test for quantitative variables, and the Chi-square test and Fishers exact test for categorical variables. A p < 0.05 was considered significant. All statistical analyses were derived using R 3.01 software.
3. Results
The study participants included 155 patients with hepatic hydatidosis. The mean age was 47.78 ± 18.34 years (52.51 ± 18.65 years in women and 40.08 ± 17.26 years in men). There was a significant difference between the mean age of women and men (p < 0.001). Sex distribution showed a female predominance (61.94% vs. 38.06%), which was statistically significant (p = 0.003). The most common symptoms were pain in the right upper quadrant and epigastrium and abdominal mass, which are shown in Table 1. A significant difference was identified between the most common symptoms (p < 0.001). Seventeen (10.97%) patients had previous surgery for hydatid disease before being referred to our center. Plain X-ray films of the abdomen showed calcification in only two (1.29%) patients, which suggests hydatid disease of the liver. The US and CT scan images demonstrated cystic lesions in most patients, which is indicative of hydatid cyst. As Table 2 demonstrates, the right lobe of the liver was the most common anatomic zone. Seventy-five (48.39%) patients had a cyst with a diameter 10 cm or greater as the greatest dimension. Five (13.16%) patients had coexisting cysts in the spleen, mesentery, and lung. The differences in cyst location and cyst diameter were significant (p < 0.001).
| Type of symptom | Frequency | % | p |
|---|---|---|---|
| Pain in the right upper quadrant and epigastrium | 119 | 76.77 | <0.001 |
| Abdominal mass | 8 | 5.16 | |
| Ascites | 18 | 11.61 | |
| Fever | 10 | 6.45 | |
| Total | 155 | 100 | |
| Location | |||
| Right lobe | 77 | 49.68 | <0.001 |
| Left lobe | 26 | 16.77 | |
| Bilaterally | 14 | 9.03 | |
| Multiple cysts in the liver | 38 | 24.52 | |
| Total | 155 | 100 | |
| Diameter category | |||
| <5 cm | 10 | 6.45 | <0.001 |
| 5–10 cm | 70 | 45.16 | |
| >10 cm | 75 | 48.39 | |
| Total | 155 | 100 | |
| Complication | Total (%) | Hospital stay (d) | Drain duration (d) | Time to return to work (d) | ||||
|---|---|---|---|---|---|---|---|---|
| Fistula | Infection of the remaining cavity | Wound infection | ||||||
| Groups | Capitonnage | 3 (3.33) | 2 (2.22) | 0 (0.00) | 5 (5.56) | 4.43 ± 2.96 | 2.10 ± 0.40 | 8.30 ± 10.40 |
| Tube drainage | 6 (9.23) | 3 (4.62) | 1 (1.54) | 10 (15.38) | 5.695 ± 3.37 | 9.20 ± 1.70 | 14.70 ± 2.30 | |
| Total | 9 (5.81) | 5 (3.23) | 1 (0.65) | 15 (9.68) | ||||
| p | 0.741 | 0.008∗ | <0.001∗ | <0.001∗ | ||||
Data are presented as n (%) or mean ± SD.
∗ The p values in bold font are statistically significant.
Based on the surgeons preference, patients were divided into two groups: tube drainage or capitonnage of the remaining cavity. The capitonnage group included 90 (58.06%) patients (67.80% male and 52.08% female). The remaining 65 (41.94%) patients (32.20% male and 47.92% female) underwent the tube drainage procedure. No significant association was found between sex and the groups (p = 0.079).
During the operation, 37 (23.87%) patients had a bile leak and 13 (8.39%) patients had a cavital infection. There was no significant blood loss. The mean operative time was 2.21 ± 0.65 hours and 2.53 ± 0.35 hours for the tube drainage group and capitonnage group, respectively, which was not significantly different (p = 0.819).
The most common complication was postoperative fistula [nine (5.81%) patients]. Postoperative infection in the remaining cavity occurred in five (3.23%) patients. Table 2 shows the postoperative complications after the two techniques. The complications in two groups were not significant (p = 0.741). For the management of postoperative fistula, two (22.22%) patients recovered without any intervention; five (55.56%) patients underwent endoscopic retrograde cholangiopancreatography and sphincterotomy; and two (22.22%) patients were lost to follow up.
The patients with cavity infection were readmitted. Samples for bacterial culture were obtained through tube drainage or through CT/US-guided percutaneous drainage. The results of culture showed Escherichia coli in three out of five patients; the other two cultures were negative. All patients were treated with ceftriaxone (2 g daily) plus metronidazole (30 mg/kg per day) and daily irrigation with normal saline. The patient with wound infection was readmitted and treated by opening the wound, daily irrigation with normal saline, and delayed closure. Other complications such as peritonitis and cholangitis did not occur. In the tube drainage group and the capitonnage group, the hospital stays were 5.695 ± 3.37 days and 4.43 ± 2.96 days, respectively (p = 0.008); drain duration, 9.2 ± 1.7 days and 2.1 ± 0.4 days, respectively (p < 0.001); and time to return to work, 14.7 ± 2.3 days and 8.3 ± 10.4 days, respectively (p = < 0.001). Cavity infection, which was managed by tube drainage, resulted in a drain duration of up to 3 weeks and consequently increased the hospital stay. In the follow-up period of 6–24 months, no recurrence of the cyst occurred.
4. Discussion
Hydatid disease is a major public health problem in developing countries. Hydatid liver disease affects all age groups and both sexes; no predisposing pathologic conditions are associated with the infection.6 According to our results, 61.94% of patients were women and 38.06% were men, and this difference was significant (p = 0.003). In accordance with other studies, the mean age is 47.78 ± 18.34 years. 7; 10 ; 11 The most common symptoms were pain in the right upper quadrant and epigastrium (76.77%) and abdominal mass (5.16%). This is also in agreement with the results of other studies. 8; 10; 11 ; 12 Ultrasonography and CT scan demonstrated cystic lesions in all patients, which suggested hydatid cysts. Plain abdominal X-ray showed calcification in only two patients, which suggested hydatid disease of the liver; however, our finding was much less common than in other reports in the literature.11 In our study, the size of cysts was the same as in previous studies. 7; 10 ; 11
Because of the high risk of cholangitis, secondary infection, rupture, and anaphylaxis, the treatment of hepatic hydatid cysts is primarily surgical; however, conservative management is preferred in older patients with small, asymptomatic, calcified cysts that are located deep in the parenchyma of the liver.6 Evacuation and irrigation of the cyst cavity is the first step in the surgical treatment of hydatid disease. During cyst evacuation, the peritoneal cavity must be carefully protected with scolocidal agents to avoid peritoneal contamination. After evacuation, the remaining cavity must be irrigated with scolocidal agents. We used 15% saline as the scolocidal agent. It has been reported that hypertonic saline solution can cause sclerosing cholangitis13; however, this complication was not observed in our series.
The second step is the management of the cystic cavity. There are several procedures for managing the cystic cavity. We compared the results of capitonnage and tube drainage. Tube drainage and capitonnage were performed in 65 (41.94%) patients and 90 (58.06%) patients, respectively, with uncomplicated cysts.
Infection of the remaining cavity was observed in five patients, which can be explained by the colonization of the accumulated fluid by ascending microorganisms in the remaining cavity. This was more correlated with the type of operation because in the tube drainage procedure the cyst cavity is not completely obliterated and accumulation of fluid is more possible.7 ; 11 The average hospital stay was shorter in patients who underwent capitonnage than in patients who underwent tube drainage (p < 0.05). This finding was confirmed and was consistent with previous studies. 8; 14; 15 ; 16 The drain duration and time to return to work were shorter in the capitonnage group than in the tube drainage group (p < 0.05). Negative cavity pressure after evacuation and irrigation by the drain alone can cause more fluid leakage through the cavity wall. The greater the fluid drainage, the greater is the drain time. Bülbüller et al 7 and Balik et al8 report peritonitis, jaundice, and biliary fistula as complications; however, peritonitis and jaundice were not identified in our study. In uncomplicated cysts, the two groups had no significant differences in the rate of postoperative complications such as biliary fistula and infection of residual cavity; however, capitonnage of the remaining cystic cavity was associated with a shorter drain duration, shorter hospital stay, and shorter time to return to work. We believe the possibility of fluid collection and biliary communication will be decreased by performing capitonnage, decreasing the dead space of the cyst cavity, and increasing the pressure inside the remaining cavity. Thus, the risk of cavity infection and biliary fistula will be decreased.
In conclusion, capitonnage and tube drainage both appear to be effective for managing the remaining cavity of hydatid cysts; however, the results of this study suggest that capitonnage is the preferred option. This procedure is not possible with a large pericyst with rigid or calcified walls. Care should be taken to prevent hepatic veins and main biliary duct injury and parenchyma tearing during deep suturing.
Acknowledgments
The results described in this paper formed part of a thesis submitted by the third author (A.H.) for a postgraduate degree in surgery. The study was supported by the Vice Chancellor for Research of Mashhad University of Medical Sciences (Mashhad, Iran). The authors gratefully acknowledge the contribution of Dr. Elena Saremi who drew the figures. We sincerely acknowledge Ms. M. Hassanpour for editing the manuscript.
References
- 1 J. Tselentis, T. Karpathios, A. Fretzayas, A. Korkas, P. Nicolaidou, N. Matsaniotis; Hydatid disease in asymptomatic young carriers in northern Greece; Am J Trop Med Hyg, 32 (1983), pp. 1462–1466
- 2 M.R. Motie, M. Ghaemi, M. Aliakbarian; Study of the radical vs. conservative surgical treatment of the hepatic hydatid cyst: a10-year experience; Indian J Surg, 72 (2010), pp. 448–452
- 3 J.K Sicklick, M.D. Angelica, Y. Fong; The Liver; C.M. Townsend, R.D. Beauchamp, B.M. Evers, K.L. Mattox (Eds.), Sabiston Textbook of Surgery (19th ed.), WB Saunders, Philadelphia (2012), pp. 1447–1449
- 4 M.R. Motie, M. Pezeshki Rad, H. Razavian, A. Rezapanah, A. Azadmand, M. Khajeh; Primary localization of a hydatid cyst in the latissimus dorsi muscle: an unusual location: a case report; Surg Infect (Larchmt), 12 (2011), pp. 401–403
- 5 D.K. Filippou, C. Kolimpiris, N. Anemodouras, S. Rizos; Modified capitonnage in partial cystectomy performed for liver hydatid disease: report of 2 cases; BMC Surg, 4 (2004), p. 8
- 6 K.K. Christians, H.A. Pitt; Hepatic abscess and cystic disease of the liver; M.J. Zinner, S.W. Ashley (Eds.), Maingots Abdominal Operations (12th ed.), McGraw-Hill, New York (2013), pp. 914–920
- 7 N. Bülbüller, Y.S. Ilhan, C. Kirkil, A. Yeniçerioğlu, R. Ayten, Z. Cetinkaya; The results of surgical treatment for hepatic hydatid cysts in an endemic area; Turk J Gastroenterol, 17 (2006), pp. 273–278
- 8 A.A. Balik, M. Başoğlu, F. Celebi, et al.; Surgical treatment of hydatid disease of the liver: review of 304 cases; Arch Surg, 134 (1999), pp. 166–169
- 9 D. Voros, D. Katsarelias, G. Polymeneas, et al.; Treatment of hydatid liver disease; Surg Infect, 8 (2007), pp. 621–627
- 10 A.K. Tsaroucha, A.C. Polychronidis, N. Lyrantzopoulos, et al.; Hydatid disease of the abdomen and other locations; World J Surg, 29 (2005), pp. 1161–1165
- 11 M.C. Safioleas, E.P. Misiakos, M. Kouvaraki, M.K. Stamatakos, C.P. Manti, E.S. Felekouras; Hydatid disease of the liver: a continuing surgical problem; Arch Surg, 141 (2006), pp. 1101–1108
- 12 C. Kayaalp, N. Sengul, M. Akoglu; Importance of cyst content in hydatid liver surgery; Arch Surg, 137 (2002), pp. 159–163
- 13 J. Belghiti, J.P. Benhamou, S. Houry, P. Grenier, M. Huguier, F. Fékété; Caustic sclerosing cholangitis; Arch Surg, 121 (1986), pp. 1162–1165
- 14 I. Sayek, R. Yalin, Y. Sanac; Surgical treatment of hydatid disease of the liver; Arch Surg, 115 (1980), pp. 847–850
- 15 S. Demirci, S. Eraslan, E. Anadol; Comparison of the results of different surgical techniques in the management of hydatid cyst of the liver; World J Surg, 13 (1989), pp. 88–90
- 16 I.D. Ozacmak, F. Ekiz, V. Ozmen, A. Isik; Management of residual cavity after partial cystectomy for hepatic hydatidosis: comparison of omentoplasty with external drainage; Eur J Surg, 166 (2000), pp. 696–699
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?