Abstract
Objectives
The aim of the study is was to determine the incidence and mortality of second hip fracture using a nationwide database.
Patients and methods
A nationwide epidemiological study was conducted using the Taiwan National Health Insurance Research Database from 2001 to 2011. Patients older than 50 years with hip fractures from 2006 to 2011 were included in the study. A total of 95,484 hip fractures were identified, with subsequent second hip fracture occurred in 4102 of them.
Results
The incidence rate ratio of second hip fracture showed a 7.13 fold of risk of further hip fracture in 3 months, 5.21 fold in one year, and remained more than 2 fold in the end of 6th year when compared with the general population. The 6-year cumulative incidence of a second hip fracture was higher in female (8.0%) than in male (6.2%). A significantly higher 1-year mortality rate was seen after a second hip fracture (18.8%) compared to the first hip fracture (14.1%) (p < 0.05). Men had higher 1- and 5-year mortality rates after second hip fractures (12.1% and 41.2%, respectively) than women (17.4% and 47.3%, respectively).
Conclusions
Patients with hip fractures would have a 2–7 fold of risk of a second fracture within 6 years. Women were more prone to a second hip fracture than men but men had a higher mortality rate.
Keywords
Second hip fracture ; Osteoporosis ; Mortality ; Geriatrics
Introduction
A fractured hip has long been recognized as a devastating event, not only for the individual, but also for the health care system.1 ; 2 Approximately 30% of patients with a hip fracture die within the first year,3 ; 4 ; 5 and many more experience significant functional loss and long-term consequences.6 ; 7
Owing to the serious socioeconomic burden of hip fractures, the incidence of hip fractures has been widely documented in different parts of the world.8 However, epidemiological analysis regarding the risk of sustaining second hip fractures is limited compared to that of sustaining the first hip fracture, as fewer studies have addressed this issue.9 ; 10 ; 11 ; 12 ; 13 ; 14 ; 15 ; 16 ; 17 ; 18
According to previous literature, the risk of a second hip fracture increases after the first one. Poorer prognosis for the second fracture compared to the first fracture has been indicated. Overall, 1- and 5-year mortality rates after a first hip fracture are 15.9% and 45.4%, respectively, while mortality rates after a second hip fracture are 24.1% and 66.5%, respectively.10 A review article in 2012 reported that the people of Taiwan, a country with approximately 23 million people, were at high risk for hip fractures.8 Therefore, the incidence and time interval of a second hip fracture should be investigated considering that the data may be useful for establishing secondary fracture preventive measures, and provide information to other countries with similar demographic structure and hip fracture incidence.
Using the Taiwan National Health Insurance Research Database (NHIRD), a nationwide database with epidemiologic information on hip fractures, the current study aimed to examine the cumulative incidences of second hip fractures according to age, sex, and time after the first hip fracture while taking competing risk of death into account. Mortality associated with second hip fractures was also assessed.
Patients and methods
Data sources
Taiwan implemented a single-payer National Health Insurance (NHI) Program in 1995 to finance health care for all residents. Enrollment in the program is mandatory for citizens, and foreigners in Taiwan are also eligible for inclusion. As of June 2012, more than 23.2 million individuals were enrolled in the NHI (coverage rate >99% of the population) and 190,885 healthcare providers contracted with NHI, representing 92.62% of all healthcare providers in Taiwan.19
The National Health Research Institute (NHRI) in Taiwan maintains the NHIRD, which contains all the claims data of the NHI program, and it provides this data to scientists for research purposes. The database comprises the following comprehensive information of insured persons: demographic data, diagnostic codes, dates of clinical visits and hospitalizations, length of hospital stay, details of prescriptions, procedures/surgeries, and expenditures.
Identification of cases
A discharge diagnosis of cervical, trochanteric, or subtrochanteric hip fractures were established on the basis of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM): 820–820.9. Cases of incident fractures were further validated by using the surgical procedure codes characteristic of a primary hip fracture surgery including hemiarthroplasty (ICD-9-CM Procedure Code 81.52) or internal fixation (ICD-9-CM Procedure Code 79.15, 79.35). Additional information such as sex, age, and overall mortality during the hospital stay were also recorded. Patients with pathological fractures (ICD-9-CM 733.14, 733.15) were excluded from the study.
A nationwide survey of hip fractures among patients aged more than 50 years between 2001 and 2011 was conducted. Patients who were admitted for a hip fracture anytime between 2001 and 2005 were excluded; therefore, we can be sure that the indexed fracture was indeed the first, as the probability of a recurrent fracture is highest the first few years following an initial fracture.20 Patients with hip fractures between 2006 and 2011, excluding those who had previous hip fractures between 2001 and 2005, were then considered as individuals with first hip fractures and included as our main subjects of analysis.
Data pertaining to a total of 120,072 hospitalizations with a hip fracture diagnosis (main or secondary) between 2006 and 2011 were obtained. We excluded 14,243 hospitalizations representing non-incident hip fractures. These included records with diagnosis codes and/or surgical procedure codes suggesting reoperation or complications (13,356 hospitalizations), or admissions occurring less than 2 weeks apart (887 hospitalizations). A total of 834 hospitalizations (0.69%) were excluded owing to missing date of admission (n = 249) or invalid/missing personal information (n = 585). Finally, 95,484 subjects with hip fractures were enrolled in the study. A patients second hospitalization with a hip fracture diagnosis code was defined as a second hip fracture if the fracture occurred more than 2 weeks after the first fracture and it was validated as an incident hip fracture (see description above). A total of 4102 subjects had second hip fractures.
Statistical analysis
The time from the first to second hip fracture, end of follow-up, or death were calculated. A cumulative incidence estimate, accounting for variable follow-up and competing risk of death, was calculated to describe the time from the first to second hip fracture for women and men separately. The analysis was repeated in 10-year age groups by using age at the first fracture. The cumulative incidence of mortality was calculated by using the Kaplan–Meier survival analysis. A log-rank test was applied to compare mortality rates following the first and second hip fracture, as well as to compare mortality rates between men and women.
IBM SPSS Statistics 20 was used for data processing and descriptive statistics. STATA 12 was used to compute cumulative incidences and perform survival analysis. Data are presented as absolute frequencies (percentages), mean ± SD, or median. The hazard ratio (HR) is presented with a 95% confidence interval (CI). The level of significance was set at 0.05.
Ethics
All researchers who plan to use the NHIRD are required to sign a written agreement declaring that the data in the NHIRD would not be used to obtain information that could potentially violate patient privacy. The study protocol was reviewed by the NHRI, who gave their agreement to the planned analysis of the NHIRD data. The present study was also approved by the Institutional Review Board (IRB) of the xxx Hospital, which is certificated by the Ministry of Health and Welfare, Taiwan.
Results
A total of 95,484 cases of first hip fractures were identified from January 1, 2006 to December 31, 2011. Among these fractures, 4102 subjects (men: 1363, women: 2739) had subsequent hip fractures in the follow-up period until December 31, 2011. The median time from the first to second fracture was 460 days for women and 465 days for men (range: 15 days to 5.9 years).
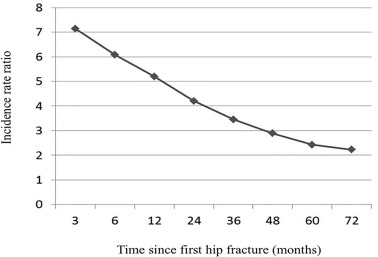
The incidence rate of a second hip fracture was 206 per 10,000 person-years for women and 174 per 10,000 person-years for men. The incidence rate ratio of a second hip fracture compared to the general population revealed that patients were 7.13 times more likely to have another hip fracture within 3 months and 5.21 times more likely to have another hip fracture within 1 year, and the rate remained more than 2 fold for within 6 years (Fig. 1 , Table 1 ).
|
|
|
Fig. 1. Incidence rate ratio of subsequent hip fracture in people with first hip fracture compared to general population. |
| Time | Incidence rate ratio | 95% confidence interval |
|---|---|---|
| 3 months | 7.13 | 7.04–7.22 |
| 6 months | 6.12 | 6.03–6.20 |
| 1 year | 5.21 | 5.14–5.28 |
| 2 years | 4.14 | 4.08–4.21 |
| 3 years | 3.51 | 3.45–3.56 |
| 4 years | 2.97 | 2.91–3.04 |
| 5 years | 2.35 | 2.30–2.40 |
| 6 years | 2.22 | 2.19–2.25 |
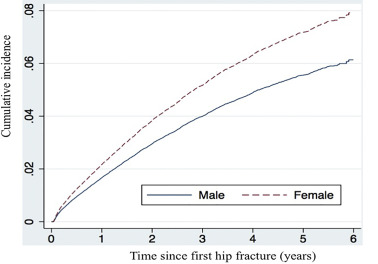
Taking the competing risk of death into account, the cumulative incidence of a second hip fracture was 2.2% for women within 1 year, 1.8% for men within 1 year, and 8.0% for women within 6 years, and 6.2% for men within 6 years (Fig. 2 , Table 2 ). The slope is the steepest in the first year following the first hip fracture in both sexes. Women demonstrated a significant propensity to have a second hip fracture compared to men 1 year after the first hip fracture (p < 0.05).
|
|
|
Fig. 2. Cumulative incidence of second hip fracture. |
| Time | Second hip fracture | a HR (women vs. men) | p -value | |
|---|---|---|---|---|
| Cumulative incidence (%) | ||||
| Women | Men | |||
| 3 months | 0.6 | 0.5 | 1.07 (0.94–1.12) | 0.447 |
| 6 months | 1.2 | 0.9 | 1.09 (0.99–1.18) | 0.091 |
| 1 year | 2.2 | 1.8 | 1.21 (1.12–1.29) | 0.018 |
| 2 years | 3.9 | 2.8 | 1.24 (1.15–1.33) | 0.003 |
| 3 years | 5.2 | 4 | 1.28 (1.20–1.36) | <0.001 |
| 4 years | 6.3 | 4.7 | 1.30 (1.21–1.39) | <0.001 |
| 5 years | 7.2 | 5.7 | 1.31 (1.24–1.39) | <0.001 |
| 6 years | 8 | 6.2 | 1.35 (1.27–1.42) | <0.001 |
a. HR, hazard ratio.
When stratified by age, the 6-year cumulative incidence revealed a significantly higher hazard ratio for women compared to men (Table 3 ), except in the age group of 50–59 years. Women and men both demonstrated the same trend of increasing incidence of a second hip fracture as they aged, which plateaued at age 70–79 years and then declined.
| Age group (years) | Women | Men | a HR (women vs. men) | p -value |
|---|---|---|---|---|
| 50–59 | 4 | 3.5 | 1.14 (0.98–1.29) | 0.441 |
| 60–69 | 7.4 | 5.8 | 1.30 (1.20–1.29) | <0.001 |
| 70–79 | 8.5 | 7 | 1.27 (1.20–1.34) | <0.001 |
| 80–89 | 8 | 6.3 | 1.26 (1.19–1.34) | <0.001 |
| ≥90 | 6.3 | 4.8 | 1.42 (1.34–1.51) | <0.001 |
a. HR, hazard ratio.
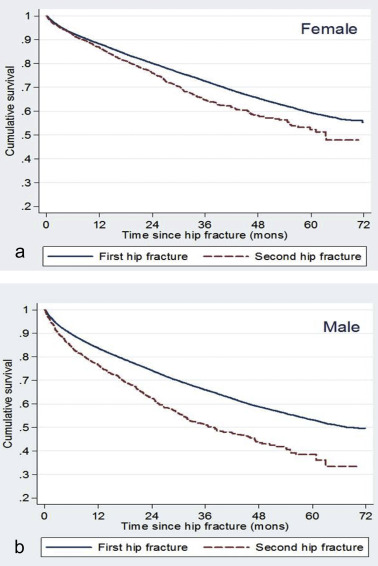
The 1- and 5-year mortality rate was 14.1% and 42% after the first hip fracture, respectively, and 18.8% and 60.6% after the second hip fracture, respectively (Fig. 3 ). Women and men both showed a significantly higher mortality rate after a second hip fracture compared to the first hip fracture 1 year after the indexed fracture (p < 0.05). When comparing differences in sex, men had a higher 5-year mortality rate than women following the first or second hip fracture (p < 0.01).
|
|
|
Fig. 3. Cumulative survival after second hip fracture. a, female. b, male. |
Discussion
Hip fracture is a major public health issue in the elderly. Taiwan, a nation of a 23 million population with majority of ethnic Chinese people, was found to have higher incidence of hip fracture than other ethnic Chinese populations, similar to that of Western countries.21 ; 22 Kanis et al reported that Taiwan was among countries with highest incidence of hip fracture, second to Scandinavian countries but higher than the UK, Germany, Hong Kong, and Singapore.8 In light of this, the present study sheds light on the epidemiologic data and mortality of second hip fracture in order to provide information for healthcare providers and policymakers in Taiwan and other countries with similar demographic structure and hip fracture incidence. In countries where population aging is just an emerging issue but is expected to accelerate rapidly in the coming decades, like China, Brazil, and southeastern Asia, our data may underestimate the incidence and mortality of second hip fractures.23 ; 24
Incidence
The current study is a nationwide population-based investigation. Most of the previous studies addressing second hip fractures involved only a small number of patients thus, limiting the power of their results.25 ; 17 ; 10 In a study from Denmark, Ryg et al reported a cumulative incidence of a second hip fracture between 1977 and 2001 of 9% within 1 year and 20% within 5 years.15 However, the incidence of a second hip fracture might be overestimated if death after the first hip fracture was not taken into account.26 In a Norwegian study, Omsland et al estimated the cumulative incidence of a second hip fracture to be 15% for women and 11% for men within 10 years of the first hip fracture, which was higher than Taiwanese population in the current study.13
The lower 1- and 5-year cumulative incidence in the present study may be caused by several reasons. First, we included younger patients aged 50–59 years who had lower risk of a second hip fracture (Table 3 ). Second, we have taken into account the competing risk of death in our analysis.13 Third, only 2.0% of the Taiwanese people aged >65 years lived in institutions according to a national survey,27 which was much lower than that in France, Australia, Japan, and Canada.28 It has been reported that living in an institution was associated with increased risk of second hip fracture because of a higher prevalence of physical disability and mental impairments.17 ; 29 ; 30 However, whether living in institutions can account for different second hip fracture incidence between countries needs further investigation, since societal factors such as government subsidies for institutionalized elderly may affect the demographic distribution of healthy or frail people. Fourth, osteoporosis is a known risk factor for hip fractures.1 ; 31 ; 32 The prevalence of osteoporosis in different study country is also an important factor to consider. The prevalence of osteoporosis was 40.8% for women aged more than 50 years and 17.7% among men in Denmark; whereas those are 12.5% and 5.3% for Chinese adults.33 ; 34 The higher osteoporosis prevalence in Nordic countries may contribute to higher incidence of second hip fractures.
In a recently published study using NHIRD in Taiwan, Shen et al analyzed cases in a 4-year period and discovered a higher one-year cumulative incidence of a second hip fracture compared to our data (4.1% and 2.7% for people aged more than 75 years and younger than 75 years, respectively).35 Death as a competing risk of a second hip fracture, however, was not taken into account in the study. In addition, patients with the diagnosis of a hip fracture within only 2 years before the index data were excluded in their study. This might not correctly identify true first hip fracture, since the incidence of second hip fracture is still high at 2 years following first hip fracture.20
Incidence rate ratio
The high incidence of a subsequent hip fracture is clustered in the first few years after the first hip fracture, as described in previous studies.20 ; 12 ; 15 In a study by Nymark et al,12 the risk of a second hip fracture diminished to a level equal to or lower than the risk of a first hip fracture after 12 months. In the current study, there was a trend toward clustering of second hip fractures in the first 6 years, but not as pronounced as described by Nymark et al. Osteoporosis prevalence in different countries may contribute to this observation, that people with more osteoporotic bones would have second hip fractures sooner.34 ; 33
Cumulative incidence according to sex
The cumulative incidence for men and women remained similar in the first 3 months and 6 months, but demonstrated a significant difference 1 year after the first hip fracture (HR, 1.21–1.35). Omsland et al found that the age-adjusted risk of a second fracture during a 10-year period was 40% higher for women compared to men.13 The authors attributed the phenomenon to the fact that the women and men have the same risk for a second hip fracture, but in general, women live longer after prior fracture, and thus, they have a higher risk for a second fracture.
When stratified by age, we found a significantly higher cumulative incidence of second fractures in women compared to men across all age groups, except for those aged 50–59 years. In this age group, there were more non-osteoporotic hip fractures, resulting in a decreased incidence of second hip fractures, and the difference between men and women was not significant.36
Mortality
The 1- and 5-year mortality rate was 14% and 42% after the first hip fracture, respectively, and 19% and 61% after the second hip fracture, respectively. The higher mortality rate after a second hip fracture may be explained by advanced age and more comorbidities. Many studies have reported mortality rates after first hip fractures.13 ; 36 ; 3 To our knowledge, only two studies have addressed the mortality rate after a second hip fracture.10 ; 15 The authors found the mortality rate after a second hip fracture remained higher compared to the first hip fracture of the similar baseline cohort. This may indicate physiologic differences in recovery following the first or second hip fracture.
When stratified by sex, the 1- and 5-year mortality rate after second hip fractures was 12.1% and 41.2% for women and 17.4% and 47.3% for men, respectively (p < 0.01). This finding was similar to previous studies. 15 ; 10 Wehren et al37 discovered a high infection rate (pneumonia/influenza and septicemia) in men after a hip fracture. This is a possible explanation for the higher mortality rate for men compared to women.
As the incidence of second hip fractures was high and the mortality rate was higher than in people with first hip fractures, it is imperative to have some interventions after the first hip fracture. Brauer et al discovered the correlation of increasing use of bisphosphonate and declining incidence of hip fracture, which suggested anti-osteoporotic treatment would decrease hip fracture rate.3 Similar finding has been reported by Alves et al that there was an abrupt turning point of hip fracture incidence and bisphosphonate use.38 Regarding treatment of osteoporosis and incidence of second hip fracture, it has been demonstrated that compliant use of bisphosphonate is effective in the prevention of second hip fractures.39 ; 40 ; 41 However, Roerholt et al found that only 9.2% of women and 4.1% of men received anti-osteoporotic therapy after a hip fracture.42 Moreover, other means of preventing fractures should be initiated along with pharmacologic therapy such as fall prevention, exercise, and use of hip protectors.43
Limitations
First, a limitation of this study is that, like other secondary databases, registration bias may occur such as a missed report or repeat registry. Second, we defined first hip fractures by excluding the hip fractures that occurred in the previous 5 years, considering that most second hip fractures happen within 5 years after the first one.20 However, there may be some patients who actually experienced a second hip fracture between 2006 and 2011 but it was considered a first hip fracture, which may decrease the overall incidence of a second hip fracture. Third, the follow-up period was moderate, leading to exclusion of some patients with subsequent hip fractures. Fourth, owing to the limitation of the database, we could not specify the fracture pattern, comorbidities, body mass index, bone marrow density, or socioeconomic status. Fifth, hip fracture patients might die before arriving at the hospital or treated in other countries. However, the numbers are most likely very small. Sixth, we did not specify those fractures due to high-energy trauma, which may have a different clinical course than an osteoporotic hip fracture. Finally, the results from current study may only apply to Taiwanese population, that may be different from other countries in osteoporosis prevalence, age distribution, societal factor, and healthcare system.
Conclusions
Patients with a hip fracture are 5–7 times more likely to suffer a second hip fracture within 1 year and twice as likely to suffer a second hip fracture within 6 years. Women were more prone to a second hip fracture compared to men; however, men had a higher mortality rate compared to women after the second hip fracture. Patients with second hip fracture show a higher mortality rate compared to first hip fracture. Due to the worldwide trend of aging and osteoporosis, efforts should be taken to prevent second hip fractures. The current study provides information to healthcare providers and policymakers in Taiwan and countries with similar demographic structure and hip fracture incidence.
Conflict of interests
The authors declare that they have no conflict of interest.
References
- 1 S.R. Cummings, L.J. Melton; Epidemiology and outcomes of osteoporotic fractures; Lancet, 359 (9319) (2002), pp. 1761–1767 http://dx.doi.org/10.1016/s0140-6736(02)08657-9
- 2 Y.I. Shyu, M.C. Chen, J. Liang, J.F. Lu, C.C. Wu, J.Y. Su; Changes in quality of life among elderly patients with hip fracture in Taiwan; Osteoporos Int, 15 (2) (2004), pp. 95–102 http://dx.doi.org/10.1007/s00198-003-1533-x
- 3 C.A. Brauer, M. Coca-Perraillon, D.M. Cutler, A.B. Rosen; Incidence and mortality of hip fractures in the United States; JAMA, 302 (2009), pp. 1573–1579 http://dx.doi.org/10.1001/jama.2009.1462
- 4 L.J. Melton, S.E. Gabriel, C.S. Crowson, A.N. Tosteson, O. Johnell, J.A. Kanis; Cost-equivalence of different osteoporotic fractures; Osteoporos Int, 14 (5) (2003), pp. 383–388 http://dx.doi.org/10.1007/s00198-003-1385-4
- 5 S.E. Roberts, M.J. Goldacre; Time trends and demography of mortality after fractured neck of femur in an English population, 1968-98: database study; BMJ, 327 (7418) (2003), pp. 771–775 http://dx.doi.org/10.1136/bmj.327.7418.771
- 6 A.G. Randell, T.V. Nguyen, N. Bhalerao, S.L. Silverman, P.N. Sambrook, J.A. Eisman; Deterioration in quality of life following hip fracture: a prospective study; Osteoporos Int, 11 (5) (2000), pp. 460–466 http://dx.doi.org/10.1007/s001980070115
- 7 S. Boonen, P. Autier, M. Barette, D. Vanderschueren, P. Lips, P. Haentjens; Functional outcome and quality of life following hip fracture in elderly women: a prospective controlled study; Osteoporos Int, 15 (2) (2004), pp. 87–94 http://dx.doi.org/10.1007/s00198-003-1515-z
- 8 J.A. Kanis, A. Oden, E.V. McCloskey, H. Johansson, D.A. Wahl, C. Cooper; A systematic review of hip fracture incidence and probability of fracture worldwide; Osteoporos Int, 23 (9) (2012), pp. 2239–2256 http://dx.doi.org/10.1007/s00198-012-1964-3
- 9 H. Hagino, T. Sawaguchi, N. Endo, Y. Ito, T. Nakano, Y. Watanabe; The risk of a second hip fracture in patients after their first hip fracture; Calcif Tissue Int, 90 (1) (2012), pp. 14–21 http://dx.doi.org/10.1007/s00223-011-9545-6
- 10 S.D. Berry, E.J. Samelson, M.T. Hannan, et al.; Second hip fracture in older men and women: the Framingham Study; Arch Intern Med, 167 (18) (2007), pp. 1971–1976 http://dx.doi.org/10.1001/archinte.167.18.1971
- 11 S.M. Kim, Y.W. Moon, S.J. Lim, et al.; Prediction of survival, second fracture, and functional recovery following the first hip fracture surgery in elderly patients; Bone, 50 (6) (2012), pp. 1343–1350 http://dx.doi.org/10.1016/j.bone.2012.02.633
- 12 T. Nymark, J.M. Lauritsen, O. Ovesen, N.D. Rock, B. Jeune; Short time-frame from first to second hip fracture in the Funen County Hip Fracture Study; Osteoporos Int, 17 (9) (2006), pp. 1353–1357 http://dx.doi.org/10.1007/s00198-006-0125-y
- 13 T.K. Omsland, N. Emaus, G.S. Tell, et al.; Ten-year risk of second hip fracture. A NOREPOS study; Bone, 52 (1) (2013), pp. 493–497 http://dx.doi.org/10.1016/j.bone.2012.09.009
- 14 T.M. Lawrence, R. Wenn, C.T. Boulton, C.G. Moran; Age-specific incidence of first and second fractures of the hip; J Bone Jt Surg Br, 92 (2) (2010), pp. 258–261 http://dx.doi.org/10.1302/0301-620x.92b2
- 15 J. Ryg, L. Rejnmark, S. Overgaard, K. Brixen, P. Vestergaard; Hip fracture patients at risk of second hip fracture: a nationwide population-based cohort study of 169,145 cases during 1977-2001; J Bone Miner Res Off J Am Soc Bone Miner Res, 24 (7) (2009), pp. 1299–1307 http://dx.doi.org/10.1359/jbmr.090207
- 16 T.K. Omsland, K. Holvik, H.E. Meyer, et al.; Hip fractures in Norway 1999-2008: time trends in total incidence and second hip fracture rates: a NOREPOS study; Eur J Epidemiol, 27 (10) (2012), pp. 807–814
- 17 E. Lonnroos, H. Kautiainen, P. Karppi, S. Hartikainen, I. Kiviranta, R. Sulkava; Incidence of second hip fractures. A population-based study; Osteoporos Int, 18 (9) (2007), pp. 1279–1285 http://dx.doi.org/10.1007/s00198-007-0375-3
- 18 H.M. Schroder, K.K. Petersen, M. Erlandsen; Occurrence and incidence of the second hip fracture; Clin Orthop Relat Res, 289 (1993), pp. 166–169
- 19 National Health Insurance in Taiwan, 2013-2014 Annual Report. http://www.nhi.gov.tw/resource/Webdata/13767_1_2013-2014NHI Annual Report.pdf .
- 20 T.A. van Geel, K.M. Huntjens, J.P. van den Bergh, G.J. Dinant, P.P. Geusens; Timing of subsequent fractures after an initial fracture; Curr Osteoporos Rep, 8 (3) (2010), pp. 118–122 http://dx.doi.org/10.1007/s11914-010-0023-2
- 21 C.J. Shao, Y.H. Hsieh, C.H. Tsai, K.A. Lai; A nationwide seven-year trend of hip fractures in the elderly population of Taiwan; Bone, 44 (1) (2009), pp. 125–129 http://dx.doi.org/10.1016/j.bone.2008.09.004
- 22 W.C. Chie, R.S. Yang, J.P. Liu, K.S. Tsai; High incidence rate of hip fracture in Taiwan: estimated from a nationwide health insurance database; Osteoporos Int, 15 (12) (2004), pp. 998–1002 http://dx.doi.org/10.1007/s00198-004-1651-0
- 23 I.J. Chen, C.Y. Chiang, Y.H. Li, et al.; Nationwide cohort study of hip fractures: time trends in the incidence rates and projections up to 2035; Osteoporos Int, 26 (2) (2015), pp. 681–688 http://dx.doi.org/10.1007/s00198-014-2930-z
- 24 U. Nations; World Population Ageing Report 2013; (2013)
- 25 A. Yamanashi, K. Yamazaki, M. Kanamori, et al.; Assessment of risk factors for second hip fractures in Japanese elderly; Osteoporos Int, 16 (10) (2005), pp. 1239–1246 http://dx.doi.org/10.1007/s00198-005-1835-2
- 26 T.A. Gooley, W. Leisenring, J. Crowley, B.E. Storer; Estimation of failure probabilities in the presence of competing risks: new representations of old estimators; Stat Med, 18 (6) (1999), pp. 695–706
- 27 Report on the Elderly Status Survey in Taiwan in 2000 (Chinese). http://sowf.moi.gov.tw/stat/Survey/89old.doc . Accessed 18.06.14.
- 28 Long Term Care Services to Older People, a Perspective on Future Needs: the Impact of an Improving Health of Older Persons. http://www.oecd.org/els/public-pensions/2429142.pdf . Accessed 12.07.14.
- 29 K.Y. Chiu, W.K. Pun, K.D. Luk, S.P. Chow; Sequential fractures of both hips in elderly patients–a prospective study; J Trauma, 32 (5) (1992), pp. 584–587
- 30 E. Guilley, T. Chevalley, F. Herrmann, et al.; Reversal of the hip fracture secular trend is related to a decrease in the incidence in institution-dwelling elderly women; Osteoporos Int, 19 (12) (2008), pp. 1741–1747 http://dx.doi.org/10.1007/s00198-008-0610-6
- 31 J.A. Kanis, O. Johnell, A. Oden, et al.; Long-term risk of osteoporotic fracture in Malmo; Osteoporos Int, 11 (2000), pp. 669–674
- 32 J.B. Lauritzen, P. Schwarz, B. Lund, P. McNair, I. Transbol; Changing incidence and residual lifetime risk of common osteoporosis-related fractures; Osteoporos Int, 3 (3) (1993), pp. 127–132
- 33 Z.Q. Zhang, S.C. Ho, Z.Q. Chen, C.X. Zhang, Y.M. Chen; Reference values of bone mineral density and prevalence of osteoporosis in Chinese adults; Osteoporos Int, 25 (2) (2014), pp. 497–507 http://dx.doi.org/10.1007/s00198-013-2418-2
- 34 L.R. Peter Vestergaard, Leif Mosekilde; Osteoporosis is markedly underdiagnosed: a nationwide study from Denmark; Osteoporos Int, 16 (2005), pp. 134–141
- 35 S.H. Shen, K.C. Huang, Y.H. Tsai, et al.; Risk analysis for second hip fracture in patients after hip fracture surgery: a nationwide population-based study; J Am Med Dir Assoc, 15 (10) (2014), pp. 725–731 http://dx.doi.org/10.1016/j.jamda.2014.05.010
- 36 L.J. Melton 3rd, D.M. Ilstrup, R.D. Beckenbaugh, B.L. Riggs; Hip fracture recurrence. A population-based study; Clin Orthop Relat Res, 167 (1982), pp. 131–138
- 37 Lois E. Wehren, W.G. Hawkes, Denise L. Orwig, J. Richard Hebel, Sheryl I. Zimmerman, Jay Magaziner; Gender differences in mortality after hip fracture: the role of infection; J Bone Miner Res Off J Am Soc Bone Miner Res, 18 (12) (2003), pp. 2231–2237
- 38 S.M. Alves, T. Economou, C. Oliveira, et al.; Osteoporotic hip fractures: bisphosphonates sales and observed turning point in trend. A population-based retrospective study; Bone, 53 (2) (2013), pp. 430–436 http://dx.doi.org/10.1016/j.bone.2012.12.014
- 39 Y.K. Lee, Y.C. Ha, B.H. Yoon, K.H. Koo; Incidence of second hip fracture and compliant use of bisphosphonate; Osteoporos Int, 24 (7) (2013), pp. 2099–2104 http://dx.doi.org/10.1007/s00198-012-2250-0
- 40 C.D. Souder, M.L. Brennan, K.L. Brennan, J. Song, J. Williams, C. Chaput; The rate of contralateral proximal femoral fracture following closed reduction and percutaneous pinning compared with arthroplasty for the treatment of femoral neck fractures; J Bone Jt Surg Am, 94 (5) (2012), pp. 418–425 http://dx.doi.org/10.2106/jbjs.j.01134
- 41 Y.K. Soong, K.S. Tsai, H.Y. Huang, et al.; Risk of refracture associated with compliance and persistence with bisphosphonate therapy in Taiwan; Osteoporos Int, 24 (2) (2013), pp. 511–521 http://dx.doi.org/10.1007/s00198-012-1984-z
- 42 C. Roerholt, P. Eiken, B. Abrahamsen; Initiation of anti-osteoporotic therapy in patients with recent fractures: a nationwide analysis of prescription rates and persistence; Osteoporos Int, 20 (2) (2009), pp. 299–307 http://dx.doi.org/10.1007/s00198-008-0651-x
- 43 G.C. Kasturi, R.A. Adler; Osteoporosis: nonpharmacologic management; PM R J Inj Funct Rehabil, 3 (6) (2011), pp. 562–572 http://dx.doi.org/10.1016/j.pmrj.2010.12.014
Document information
Published on 31/03/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?