Summary
Background
The purpose of this study was to determine whether the mucosal expression of interleukin (IL)-23p19 has a role in the pathogenesis of ulcerative colitis, and to determine its relation to disease severity.
Methods
This study was performed on 50 patients with ulcerative colitis and 10 normal individuals as the controls. They were divided into Group I (27 patients with mild to moderate disease), Group II (23 patients with severe disease), and Group III (10 normal individuals). All patients and the controls were subjected to histopathological study, IL-23p19 immunohistochemical staining, IL-23R expression by flow cytometry, and serum IL-23 by enzyme-linked immunoassay.
Results
There was a significant increase in IL-23p19 gene expression and IL-23R level in patients with ulcerative colitis, compared to the controls. A significant positive correlation was detected between increased expression of the IL-23p19 gene, IL-23R, high serum IL-23, and the severity of the disease.
Conclusion
Increased expression of the IL-23p19 gene has a role in the pathogenesis of ulcerative colitis. Targeted therapy directed against IL-23p19 may be effective in its treatment. Increased expression of the IL-23p19 gene and IL-23R with high serum IL-23 is correlated positively with disease severity.
Keywords
Interleukin 23p19 gene ; Interleukin-23 R expression ; Ulcerative colitis
Introduction
Inflammatory bowel disease consists of two distinct diseases: Crohns disease (CD) and ulcerative colitis (UC). Both diseases may arise because of the combination of genetic variations and alterations in bacterial flora that can subsequently drive a dysregulated immune response that results in chronic intestinal inflammation [1] ; [2] .
Interleukin (IL)-23 is a member of a small family of proinflammatory cytokines, consisting of a p19 subunit and a common p40 subunit that is shared with IL12 [3] . The receptor for IL-23 (IL-23R) consists of the IL-12R beta 1 subunit and a novel component termed “IL-23R” [4] , which is expressed predominantly on T cells, natural killer (NK) cells, and natural killer T (NKT) cells, and to a smaller extent on monocytes, macrophages, and dendritic cells (DCs) [5] . Interleukin 23 has a crucial role in the pathogenesis of several immune-mediated inflammatory diseases by recruiting several inflammatory cells and Th17 cells [6] ; [7] . Interleukin 23 promotes Th17 cells in producing tumor necrosis factor alpha (TNFα), IL-17, IL-6, IL-22, granulocyte-macrophage colony-stimulating factor, and other novel factors, which are associated with the induction of autoimmune inflammation [6] ; [8] ; [9] . This study was performed to determine whether the mucosal expression of IL-23p19 has a role in the pathogenesis of UC and to elucidate its relation to disease severity.
Materials and methods
Patients and methods
This study was performed on 50 patients with UC and 10 individuals (i.e., the controls) for whom colonoscopic and histopathologic findings were normal. This study was accepted by the medical ethics committee of the Faculty of Medicine at Tanta University (Tanta, Egypt). Each patient provided written consent after they received a complete explanation of the protocol of the study. The studied patients were selected from the inpatient and outpatient clinics of the Tropical Medicine and Internal Medicine Departments of the Tanta University Hospital (Tanta, Egypt) in the period between November 2012 and October 2013. Ulcerative colitis patients were diagnosed on the basis of clinical, endoscopic, and histological manifestations according to the criteria of the American Gastroenterology Association [10] . The patients were divided, based on endoscopic and histopathological findings, into Group I (27 patients with mild to moderate UC disease), Group II (23 patients with severe UC disease), and Group III (10 individuals whose colonoscopic and histopathologic findings were normal as control). Patients in the following categories were excluded from the study: patients who were pregnant; patients who had a malignancy, heart failure, renal failure, thyroid disorders, acute infection, or stroke; and patients taking immunosuppressive drugs.
All patients and controls were subjected to a complete history taking and thorough clinical examination. Laboratory investigations such as complete blood picture, blood urea and serum creatinine, erythrocyte sedimentation rate, and stool examination were performed to exclude bacterial causes of colitis. Colonoscopy was performed in all groups and the severity of the disease was determined. The endoscopic scoring system for UC by Pineton de Chambrun et al [11] was used, as follows: Score 0, normal or inactive disease; Score 1, mild disease (i.e., erythema, decreased vascular pattern, and mild friability); Score 2, moderate disease (marked erythema, increased vascular pattern, friability, and erosion); and Score 3 (severe disease with spontaneous bleeding and ulceration). Endoscopic findings were recorded and multiple biopsies were obtained for histopathology, IL-23p19 immunohistochemical staining, and IL-23 R expression by flow cytometry.
Histopathological study
Four-micrometer thick serial sections of formalin fixed, paraffin-embedded tissue were cut and stained using hematoxylin and eosin for histopathological evaluation and grading of the groups. A six grade classification system for inflammation was used. The grades were: 0, structural change only; 1, chronic inflammation; 2, lamina propria neutrophils; 3, neutrophils in the epithelium; 4, crypt destruction; and 5, erosions or ulcers [12] .
Interleukin-23p19 immunohistochemical staining
Four-micrometer thick serial sections of formalin fixed, paraffin-embedded tissue were cut and mounted on positively charged glass slides. After incubation at 60°C overnight and deparaffinization, the sections were placed in 0.01M sodium citrate buffer (pH 6.0) and heated twice for 5 minutes in a microwave oven. After inactivation of endogenous peroxidase with 0.5% metaperiodic acid in phosphate-buffered saline (PBS) for 10 minutes, the sections were incubated with 10% horse serum in PBS for 1 hour. The sections were then incubated at 4°C overnight with 100× diluted primary goat antimouse IL-23p19 antibody (R&D Systems, Inc., Minneapolis, MN, USA). The standard avidin–biotinperoxidase complex (ABC) technique was performed using the LabVision Secondary Detection Kit (UltraVision Detection System Anti-polyvalent, HRP). The color was visualized by incubation with chromogen 3,3′-diaminobenzidine for 5 minutes. The slides were then counterstained with Mayer hematoxylin and cover slipped with Permount (StatLab, McKinney, TX). Negative controls without the primary antibodies were set for each test.
Immunohistochemical evaluation
Results were expressed semiquantitatively. Positively stained cells were counted by examining at least 10 random fields (200×) in each section and expressed as the percentage of positive cells over the total cell number [13] .
IL-23R expression by flow cytometry
Peripheral blood mononuclear cells
Lymphocytes were isolated from peripheral blood by incubation with Rosette Sep Human CD4+T cells (cytotoxic T-lymphocytes) enrichment cocktail (Stem Cells Technologies, Grenoble, France), followed by centrifugation on a density gradient (Lymphoprep; PAA, Pasching, Austria). Lymphocytes were purified by centrifugation through Lymphoprep.
Peripheral CD4+
For cellular surface staining the following antibodies and secondary reagents were used in different combinations: biotinylated goat antihuman IL-23R (BAF1400; R&D Systems). Streptavidin-APC (BD Bioscience, San Jose, CA, USA), CD3-FITC (eBioscience, San Diego, CA, USA), CD4 PE-Texas Red (Invitrogen, Carlsbad, CA, USA), CD45RO-FITC (Dako, Glostrup, Denmark), CD45RO-Pacific Blue (BioLegend, San Diego, CA, USA), CCR6-PE (BD Bioscience), CD45RA-PE (Invitrogen), CD45RA-PE-Cy7 (eBioscience), plus matched isotypes as controls. Cells were acquired on a BD FACSAria II (BD Bioscience). Analysis of fluorescence-activated cell sorting (FACS) data was performed using FlowJo software (TreeStar, Ashland, OR. USA).
Lamina propria mononuclear cells
Isolation of intestinal lymphocytes
For intraepithelial lymphocytes (IEL) isolation, endoscopic procedure was performed as follows: intestinal tissue were removed and washed through with cold CMF using a 50 mL syringe fitted with a short plastic cannula. This removed all food remains and most mucus. The cleaned intestines were then placed on CMF-moistened paper towels. After addition of EDTA in CMF, the guts were incubated at room temperature with a magnetic stirrer to remove the epithelium. When the supernatant fluid became sufficiently clouded with cells, it was removed and fresh EDTA/CMF added (usually every 15 minutes). After approximately 90 minutes, no more cells were seen in the supernatant, which indicated that all of the epithelium had been removed. This was confirmed by histological examination of the remaining fragments. The pieces were then washed with CMF and incubated for 20 minutes with stirring in 25 mL RPMI/NCS to inactivate any remaining EDTA. The remaining fragments were then transferred to flasks containing 15 mL RPMI/NCS containing collagenase. The flasks and contents were then incubated at 37°C in an orbital incubator (Gallenkamp typeIH 460) for 90 minutes at 180 cycles/min.
The supernatant from each wash was pooled and poured through a nylon wool column to enrich T cells and remove the mucus. The resulting cell suspension was used to analyze IEL.
Intraepithelial lymphocytes
The IEL suspensions containing approximately 1 × 105 cells each were resuspended in cold PBS and stained with Aqua Live/Dead cell discriminator (Invitrogen; catalog no. L34597) in accordance with the manufacturers protocol. Cells were then stained for 1 hour in the dark at 4°C with optimized concentrations of anti-CD3 Alexa750-APC (eBioscience; clone 17A2), anti-CD8 Alexa700 (eBioscience; clone 53-6.7), anti-CD4 Pacific Blue (eBioscience; clone RM4-5), anti-TCR GD R-PE (BD Bioscience; Pharmingen clone GL3), and biotinylated polyclonal anti-IL-23R (BAF1686; R&D Systems). Cells were washed twice with PBS containing 1% bovine serum albumin (FACS) buffer). Cells were then stained for 1 hour with streptavidin-conjugated Qdot 605 (Q10101MP; Invitrogen). Stained cells were washed once in FACS buffer and subsequently fixed in 4% formalin for 1 hour. The cells were then washed once and resuspended in FACS buffer and analyzed using an LSR II flow cytometer (Becton Dickinson, San Jose, CA). The data were analyzed by using FlowJo software (Treestar, Inc., Ashland, OR). Gates were set on singlets and then on live lymphocytes. Subsequent gates were based on Fluorescence-Minus-One and unstained controls.
Serum IL-23 by enzyme-linked immunosorbent assay
IL-23 cytokine level was assayed using a commercially available IL-23 enzyme-linked immunosorbent assay (ELISA) kit (R&D Systems) according to the manufacturer’s instructions.
Statistical analysis
The statistical data are reported as the mean ± standard deviation (SD), frequencies (number), and percentages when appropriate. A comparison of numerical variables between the study groups was performed using Mann–Whitney U test to compare independent samples from the two groups. The one-way analysis of variance test was used to compare between more than two groups when the data were normal and the Kruskal–Wallis test was used when the data were not normal. Qualitative data was compared using the Chi-square test. Spearman’s rank correlation was used to quantify the association between continuous or ordered categorical variables. A p < 0.05 was statistically significant. All statistical calculations were performed using the computer program SPSS version 15 for Microsoft Windows (Statistical Package for the Social Science; SPSS, Chicago, IL, USA).
Results
Clinical and laboratory data of the studied groups
Significantly higher levels of ESR and disease duration were detected in patients with severe disease, compared to patients with mild to moderate UC disease (p < 0.05). Abdominal pain, diarrhea, blood in the stool, and ESR were significantly higher in UC patients, compared to the controls ( Table 1 ).
| Parameters | Mild to moderate UC Group I (n = 27) | Severe UC Group II (n = 23) | Control Group Group III (n = 10) | p |
|---|---|---|---|---|
| Age (y) | 36.1 ± 13.4 | 41.5 ± 12.7 | 35.2 ± 12.8 | 0.270 |
| Sex (m/f) | 16/11 | 14/9 | 6/4 | 1.000 |
| Disease duration (y) | 2.6 ± 1.7 | 4.2 ± 3.1 a | — | 0.042 a |
| Abdominal pain | 20/27 | 18/23 | 3 b | 0.083 |
| Diarrhea | 18/27 | 19/23 | 2 b | 0.017 * |
| Blood in stool | 19/27 | 21/23 | — | 0.111 |
| ESR (mm/h) | 21.8 ± 7.9 | 33.6 ± 8.5 a | 10.9 ± 1.9 b | <0.001 * |
| Hb (gm/d) | 12.1 ± 1.3 | 11.6 ± 1.6 | 12.6 ± 1.5 | 0.197 |
- Indicates p < 0.05 between all groups.
Group I, patients with mild to moderate disease; Group II, severe disease; Group III, no disease (normal control).
UC = ulcerative colitis; ESR = erythrocyte sedimentation rate; Hb = hemoglobin.
a. Significant difference between Group I and Group II.
b. Significant difference between patients and the controls.
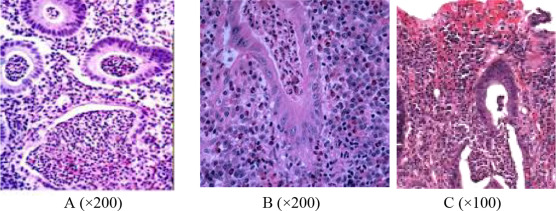
Histopathological evaluation and correlation with endoscopic groups
The 50 studied patients with UC showed different grades of severity: 5 (10%) patients were Grade 0; 12 (24%) patients were Grade 1; 8 (16%) patients were Grade 2; 15 (30%) patients were Grade 3 (Figure 1 A); 6 (12%) patients were Grade 4 (Figure 1 B); and only four (8%) patients were Grade 5 (Figure 1 C). In correlation with the endoscopic grouping, the Group I patients were distributed among Grades 0–3, whereas the Group II patients were distributed among Grades 2–5 with statistical significance (p = 0.02) ( Table 2 ).
|
|
|
Figure 1. Histopathological grades of ulcerative colitis shows (A) Grade 3, neutrophilic infiltrate in the epithelial cells; (B) Grade 4, crypt destruction; and (C) Grade 5, erosions and ulcers (hematoxylin and eosin stain). |
| Studied groups | Histopathological grading | p | |||||
|---|---|---|---|---|---|---|---|
| Grade 0 | Grade 1 | Grade 2 | Grade 3 | Grade 4 | Grade 5 | ||
| Mild to moderate UC Group I (n = 27) | 5 | 12 | 6 | 4 | 0 | 0 | 0.02 * |
| Severe UC Group II (n = 23) | 0 | 0 | 2 | 11 | 6 | 4 | |
- Indicates a significant value, p < 0.05.
Group I, patients with mild to moderate disease; Group II, severe disease; Group III, no disease (normal control).
IL-23 R expression, serum IL-23 and IL-23p19 expression in the studied groups
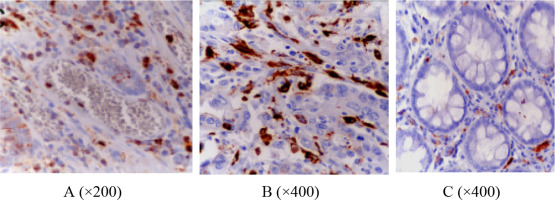
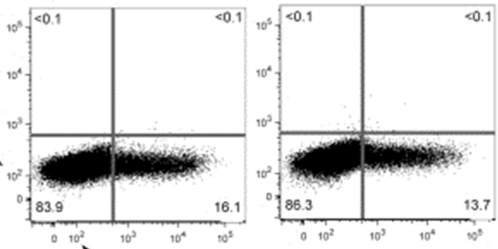
Table 3 shows a significant increase in the serum level of IL-23 and IL-23R expression in peripheral blood and in lamina propria lymphocyte (CD4) in the UC patient group, compared to the control group. This increase was greater in patients with severe disease, compared to patients with mild to moderate disease. Immunohistochemical evaluation of IL-23p19 showed that was expressed in the lamina propria macrophages. The mean number of cells expressing IL-23p19 in Group I was 11.6 ± 3.4 (Figure 2 A) and in Group II was 19.6 ± 5.5 (Figure 2 B). The difference was statistically different between the two groups. By contrast, the number of cells was only 3.5 ± 1.6 in Group III (i.e., the control group; Figure 2 C). The difference between the three groups was statistically significant. Based on flow cytometry analysis, IL-23R was highly expressed in the severe lesions in Group II, compared to its expression in the mild lesions in Group I (Figure 3 ; Figure 4 ); this difference is highly statistically significant.
| Parameters | Mild to moderate UC Group I (n = 27) | Severe UC Group II (n = 23) | Control group Group III (n = 10) | p |
|---|---|---|---|---|
| IL-23 R expression % | ||||
| PBMC | 6 | 12 | 1 | 0.037 * |
| LPMC | 20 | 29 | 6 | 0.001 * |
| S IL-23 (pg/mL) | 48.9 ± 7.6 | 137.4 ± 45.5 | 24.2 ± 9.4 | <0.001 * |
| IL-23 p 19 expression Immunohistochemistry % of +ve cells | 11.6 ± 3.4 | 19.6 ± 5.5 | 3.5 ± 1.6 | <0.001 * |
- Indicates p < 0.05, between all groups.
Group I, patients with mild to moderate disease; Group II, severe disease; Group III, no disease (normal control).
IL = interleukin; LPMC = lamina propria mononuclear cells (i.e., lymphocytes); PBMC = peripheral blood mononuclear cells (i.e., lymphocytes); UC = ulcerative colitis.
|
|
|
Figure 2. Immunohistochemical expression of IL23p19 in the ulcerative colitis groups shows (A) mild expression in Group I, (B) extensive expression in Group II, and (C) very minimal expression in Group III. |
|
|
|
Figure 3. In PBMC and LPMC, IL23R is mildly increased in Group I. IL = interleukin; LPMC = lamina propria mononuclear cell; PBMC = peripheral blood mononuclear cell. |
|
|
|
Figure 4. In PBMC and LPMC, IL23R is highly increased in Group II. IL = interleukin; LPMC = lamina propria mononuclear cell; PBMC = peripheral blood mononuclear cell. |
Correlation between endoscopic severity, histopathological grading, and studied parameters in UC patients
Table 4 shows a significant positive correlation between endoscopic severity and histological grading of UC with IL-23p19 expression (r = 0.591, p = 0.038; and r = 0.612, p = 0.047, respectively), IL-23R expression (r = 0.542, p = 0.015; and r = 0.526, p = 0.031, respectively), and serum level of IL-23 (r = 0.637, p = 0.024; and r = 0.551, p = 0.019, respectively).
| Parameters | IL-23p19 expression | IL-23 R expression | Serum IL-23 | |||
|---|---|---|---|---|---|---|
| R | p | R | p | R | p | |
| Endoscopic severity | 0.591 | 0.038 * | 0.542 | 0.015 * | 0.637 | 0.024 * |
| Histopathological grade | 0.612 | 0.047 * | 0.526 | 0.031 * | 0.551 | 0.019 * |
- Indicates p < 0.05.
IL = interleukin; UC = ulcerative colitis.
Discussion
Patients with UC are at increased risk of inflammation. Interleukin-23 is a newly identified cytokine with increased expression in inflamed biopsies of colon mucosa in patients with CD; however, there is inconsistent evidence on its role in UC [14] . Interleukin-23 is a heterodimeric cytokine that shows similar function as IL-12 in promoting cellular immunity and enhancing lymphocyte proliferation [15] .
This study showed significant increased expression of the IL-23p 19 gene in patients with UC, compared to the controls. This increase was significantly higher in patients with severe UC disease, compared to patients with mild to moderate disease. This was similar to the results reported by Schmidt et al [16] , Zhanju et al [13] , and Kobayashi et al [17] . We observed that, based on immunohistochemistry, IL-23p19-positive cells were primarily macrophages. This was in agreement with the findings of Zhanju et al [13] . These findings suggest that IL-23 is produced by intestinal mucosal macrophages in the inflamed mucosa of UC patients [13] . On stimulation by bacterial ligand, IL-23 is produced by antigen-presenting cells. After binding to an appropriate receptor (i.e., IL-23R), this cytokine can stimulate the production of IL-17, TNFα, and IL-6 from T cells. Interleukin-17 stimulates the expression of adhesion molecules such as ICAM-1 on endothelial cells, and stimulates the release of IL-6 and IL-8 from myofibroblast and epithelial cells. Interleukin-8 acts as a chemotactic factor for neutrophil influx into the intestines. Inflammatory neutrophils release inflammatory mediators such as matrix metalloproteinase and inducible nitric oxide. This sequelae of pathogenic events lead to the chronic inflammation and epithelial cell damage associated with the disease [18] . Therefore, IL-23 was proposed to have an integral role in the pathogenesis of inflammatory bowel disease [19] .
The present study showed increased expression of IL-23R in the peripheral blood and in the mucosal biopsy of samples from UC patients was significant, compared to the control group. This increased expression was higher in patients with severe disease, compared to patients having mild to moderate disease. In addition, Zhanju et al [13] demonstrated significant increased expression of IL-23R in the peripheral blood and mucosal lamina propria cells.
In accordance with the findings reported by Mohammadi et al [14] and Zheng et al [20] , we demonstrated increased serum level of IL-23 in UC patients, compared to the controls. In addition, the increased serum levels of IL-23 were greater in patients with severe disease than in patients with mild to moderate disease. Furthermore, this study reported a significant positive correlation between high serum IL-23 levels and endoscopic severity of the disease. These findings support the hypothesis that, increased IL-23 levels reflect the activity of T helper 17 cells in patients with UC and that IL-23 participates in the pathogenesis of the disease [20] . In the current study, the increased expression of IL-23p19 and IL-23 R were significantly and positively correlated with the endoscopic severity of the disease. These were consistent with the findings of Schmidt et al [16] and Zhanju et al [13] . In agreement with experimental studies of Daniel et al [21] and Ando et al [22] , there was a significant positive correlation between histopathological severity and the expression of IL-23p19 and IL-23R in the mucosa of UC patients. Furthermore the severity of histopathological lesions was significantly correlated with serum IL-23, a finding that was similar to the findings of an experimental study by Sheikh et al [23] .
We conclude that the increased expression of IL-23p19 has a role in the pathogenesis of UC; therefore, targeted therapy directed against IL-23p19 may have a therapeutic role in treating the disease. The increased expression of IL-23p19, IL-23R, and serum IL-23 are correlated with disease severity. A limitation of this study was the small number of the patients. Further studies on a larger population and on patients under treatment are needed.
Conflicts of interest
All authors declare no conflicts of interest.
References
- [1] D.Q. Shih, S.R. Targan; Insights into IBD pathogenesis; Curr Gastroenterol Rep, 11 (2009), pp. 473–480
- [2] M. Nagahori, Y. Nemoto, M. Watanabe; Pathogenesis of inflammatory bowel disease; Intest Res, 8 (2010), pp. 9–17
- [3] B. Oppmann, R. Lesley, B. Blom, J.C. Timans, Y. Xu, B. Hunte, et al.; Novel p19 protein engages IL-12p40 to form cytokine, IL-23, with biological activities similar and distinct from IL-12; Immunity, 13 (2000), pp. 715–725
- [4] C. Parham, M. Chirica, J. Timans, E. Vaisberg, M. Travis, J. Cheung, et al.; A receptor for the heterodimeric cytokine IL-23 is composed of IL-12Rbeta1 and a novel cytokine receptor subunit, IL-23R; J Immunol, 168 (2002), pp. 5699–5708
- [5] Y. Zheng, D.M. Danilenko, P. Valdez, I. Kasman, J. Eastham-Anderson, J. Wu, et al.; Interleukin-22, a T (H) 17 cytokine, mediates IL-23-induced dermal inflammation and acanthosis; Nature, 445 (2007), pp. 648–651
- [6] C.L. Langrish, Y. Chen, W.M. Blumenschein, J. Mattson, B. Basham, J.D. Sedgwick, et al.; IL-23 drives a pathogenic T cell population that induces autoimmune inflammation; J Exp Med, 201 (2005), pp. 233–240
- [7] T. Korn, E. Bettelli, M. Oukka, V.K. Kuchroo; IL-17 and Th17 cells; Annu Rev Immunol, 27 (2009), pp. 485–517
- [8] F.M. Brennan, I.B. McInnes; Evidences that cytokines play a role in rheumatoid arthritis; J Clin Invest, 118 (2008), pp. 3537–3541
- [9] S. Hue, P. Ahern, S. Buonocore, M.C. Kullberg, D.J. Cua, B.S. McKenzie, et al.; Interleukin-23 drives innate and T cell-mediated intestinal inflammation; J Exp Med, 203 (2006), pp. 2473–2483
- [10] A. Kornbluth, D.B. Sacher; Ulcerative colitis practice guidelines in adult: American College of Gastroenterology, Practice Parameters Committee; Am J Gastroenterol, 105 (2010), pp. 501–523
- [11] G. Pineton de Chambrun, L. Peyrin-Biroulet, M. Lémann, J.F. Colombel; Clinical implication of mucosal bealing for the management of IBD; Nat Rev Gastroenterol Hepatol, 7 (2010), pp. 15–29
- [12] K. Geboes, R. Riddell, A. Ost, B. Jensfelt, T. Persson, R. Löfberg; A reproducible grading scale for histological assessment of inflammation in ulcerative colitis; Gut, 47 (2000), pp. 404–409
- [13] Z. Liu, P.K. Yadav, X. Xu, J. Su, C. Chen, M. Tang, et al.; The increased expression of IL-23 in inflammatory bowel disease promotes intraepithelial and lamina propria lymphocyte inflammatory responses and cytotoxicity; J Leukoc Biol, 89 (2011), pp. 597–606
- [14] M. Mohammadi, M.M. Hayatbakhsh, M.J. Zahedi, M.R. Jalalpour, A. Pakgohar; Serum interleukin-23 levels in patients with ulcerative colitis; Iran J Immunol Sept, 8 (2011), pp. 183–188
- [15] S. Aggarwal, N. Ghilardi, M.H. Xie, F.J. de Sauvage, A.L. Gurney; Interleukin-23 promotes a distinct CD4 T cell activation state characterized by the production of interleukin-17; J Biol Chem, 278 (2003), pp. 1910–1914
- [16] C. Schmidt, T. Giese, B. Ludwig, I. Mueller-Molaian, T. Marth, S. Zeuzem, et al.; Expression of interleukin-12-related cytokine transcripts in inflammatory bowel disease: elevated interleukin-23p19 and interleukin-27p28 in Crohns disease but not in ulcerative colitis; Inflamm Bowel Dis, 11 (2005), pp. 16–23
- [17] T. Kobayashi, S. Okamoto, T. Hisamatsu, N. Kamada, H. Chinen, R. Saito, et al.; IL-23 differentially regulates Th1/Th17 balance in ulcerative colitis and Crohns disease; Gut, 57 (2008), pp. 1682–1689
- [18] L.R. Fitzpatrick; Novel pharmacological approaches for inflammatory bowel disease: targeting key intracellular pathway and the IL-23/IL-17 axis; Intern J Inflamm, 10 (2012), pp. 1–8
- [19] D. McGovern, F. Powrie; The IL-23 axis plays a key role in the pathogenesis of IBD; Gut, 56 (2007), pp. 1333–1336
- [20] Z.D. Zheng, X.O. Wan, L.Y. Liu; Serum contents of IL-23 and IL-17 in the patients with ulcerative colitis and the clinical significance; Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi, 27 (2011), pp. 203–206
- [21] C. Daniel, N.A. Sartory, N. Zahn, H.H. Radeke, J.M. Stein; Immune modulatory treatment of trinitrobenzene sulfonic acid colitis with calcitrol is associated with change of T helper (TH) 1/Th17 to a Th2 and regulatory T cell profile; J Pharmacol Exp Ther, 324 (2008), pp. 23–33
- [22] Y. Ando, G.X. Yang, M. Tsuda, K. Kawata, W. Zhang, T. Nakajima, et al.; The immunobiology of colitis and cholangitis in interleukin-23p19 and interleukin-17A deleted dominant negative form of transforming growth factor beta receptor type II mice; Hepatology, 56 (2012), pp. 1418–1426
- [23] S.Z. Sheikh, K. Matsuoka, T. Kobayashi, F. Li, T. Rubinas, S.E. Plevy; Cutting edge: IFN-gamma is a negative regulator of IL-23 in murine macrophages and experimental colitis; J Immunol, 184 (2010), pp. 4069–4073
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?